Blood Clot After Stent – What You Need to Know
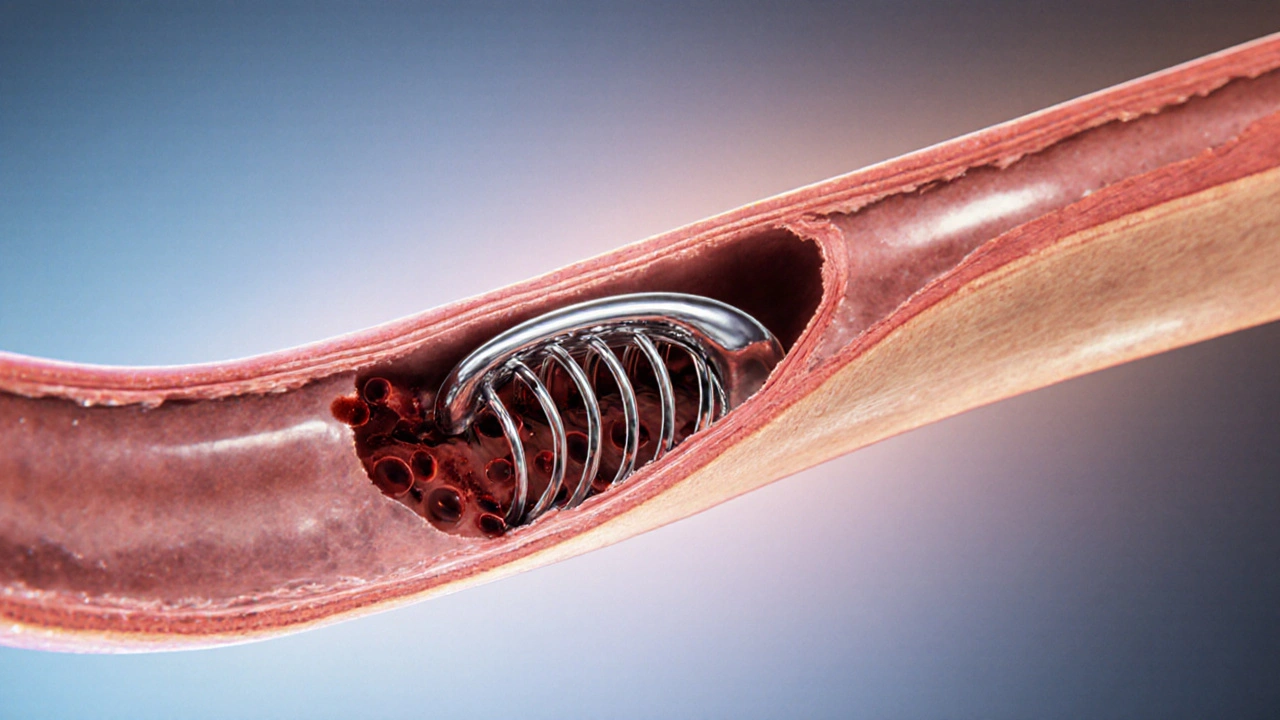
When dealing with blood clot after stent, a blockage caused by a clot forming on a coronary stent after placement. Also known as stent thrombosis, it can turn a life‑saving procedure into a serious emergency.
The first thing to understand is that a stent, a tiny mesh tube placed in a narrowed artery to keep it open is a foreign object. Your body’s natural response is to send platelets to the site, which can lead to clot formation if the right checks aren’t in place. This is why blood clot after stent management hinges on two key actions: preventing clotting and monitoring the artery. Anticoagulation therapy and dual antiplatelet therapy are the main weapons doctors use.
Key Factors & Treatments
Effective anticoagulation, medication that reduces the blood’s ability to form clots is essential for patients with high clot risk, especially those with atrial fibrillation or previous clot events. Anticoagulation works by interrupting the clotting cascade, lowering the chance that a clot will lock onto the stent surface. At the same time, dual antiplatelet therapy (DAPT), the combined use of aspirin and a P2Y12 inhibitor targets platelet activation, a separate pathway that also contributes to stent thrombosis. Together, these treatments form a two‑pronged defense: anticoagulation blocks clotting factors, while DAPT keeps platelets from sticking.
Beyond meds, the underlying condition matters. Most people who get stents have coronary artery disease (CAD), the buildup of plaque in heart arteries. CAD drives inflammation, and inflamed vessels are more likely to develop clots. Lifestyle changes—like quitting smoking, eating heart‑healthy foods, and staying active—reduce inflammation and complement medical therapy. Regular follow‑up imaging, such as an angiogram or CT scan, helps catch early signs of restenosis or clot formation before they become critical.
When a clot does form, swift action is critical. Interventional cardiologists may perform a repeat angiography to locate the blockage, then use thrombectomy devices or additional stenting to restore flow. In many cases, they will intensify anticoagulation or switch to a more potent P2Y12 inhibitor for a short period. The goal is to dissolve the clot, prevent recurrence, and keep the artery open for the long term.
Understanding the links between stent placement, clot risk, and the therapies that control them gives you a solid foundation. Below you’ll find articles that dive deeper into each of these pieces— from how specific drugs like saxagliptin affect kidney function in diabetic patients with stents, to the role of pulmonary rehab for asthma sufferers who also face heart disease. Whether you’re a patient, a caregiver, or just curious, the collection offers practical tips, real‑world evidence, and clear guidance to help you navigate the complex world of blood clot after stent.
How Exercise Helps Prevent Blood Clots in Stents
Learn how regular exercise lowers the risk of blood clots in coronary stents, what types of activity work best, and how to combine workouts with medication safely.