Inhaled Steroid Comparison Tool
Recommended Inhaled Steroid
Potency:
Typical Dose:
Dosing Frequency:
FDA Approval:
Common Side Effects
Why This Recommendation?
Quick Reference Guide
| Drug | Potency | Dosage | Dosing | Side Effects |
|---|---|---|---|---|
| Beclomethasone Dipropionate | 1× (reference) | 200-800 µg | Twice daily | Oral thrush, hoarseness |
| Fluticasone Propionate | 1.5× | 100-500 µg | Once or twice daily | Thrush, possible systemic cortisol suppression |
| Budesonide | 0.8× | 200-800 µg | Twice daily | Thrush (lower incidence), mild systemic effects |
| Mometasone Furoate | 2× | 50-200 µg | Once daily | Thrush, dysphonia |
| Ciclesonide | 1× (after activation) | 80-320 µg | Once or twice daily | Lowest oral thrush rates, mild hoarseness |
When you or someone you care about needs a daily inhaled steroid, the sheer number of brand‑name and generic options can feel overwhelming. Beclomethasone Dipropionate is a staple in many asthma and COPD action plans, but it isn’t the only player on the field. This guide walks through the most common alternatives, highlights the key data you’ll want to compare, and offers a quick‑reference checklist so you can decide which inhaled corticosteroid (ICS) fits your lifestyle and medical needs.
Key Takeaways
- Beclomethasone Dipropionate provides moderate potency with twice‑daily dosing for most patients.
- Fluticasone Propionate and Mometasone Furoate deliver higher potency, often allowing once‑daily use.
- Budesonide’s lower systemic absorption makes it a good choice for patients worried about bone density.
- Ciclesonide activates only after inhalation, reducing oral thrush risk.
- Choosing the right ICS involves weighing potency, dosing frequency, side‑effect profile, and cost.
Understanding Inhaled Corticosteroids
Inhaled corticosteroid is a class of anti‑inflammatory drugs delivered directly to the lungs to control chronic airway diseases such as asthma and chronic obstructive pulmonary disease (COPD). They work by reducing airway swelling, mucus production, and hyper‑responsiveness, which translates into fewer flare‑ups and better daily breathing. Most guidelines recommend starting with a low‑to‑moderate dose and stepping up only if control remains inadequate.
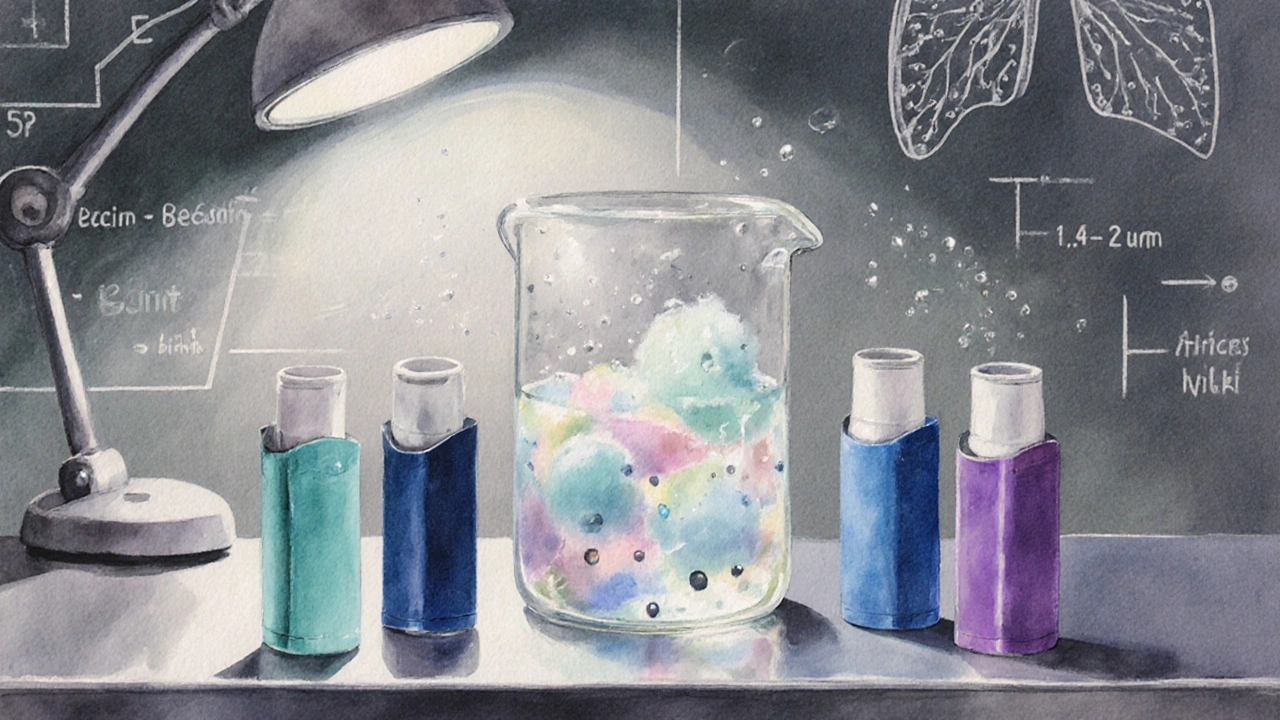
Beclomethasone Dipropionate - The Baseline
Beclomethasone Dipropionate is a synthetic glucocorticoid formulated as an inhalation aerosol or dry‑powder inhaler (DPI), first approved by the FDA in 1975. It offers moderate potency, typically prescribed in doses ranging from 100 to 400 µg twice daily. Common brand names include Qvar and Beclovent. The drug’s particle size (1.5‑2.5µm) allows deep lung penetration, but because it’s a pro‑drug, activation occurs in the airway epithelium, limiting systemic exposure.
Side effects you’ll hear about most often are oral thrush, hoarse voice, and a slight increase in intra‑ocular pressure for susceptible individuals. For many patients, the twice‑daily schedule fits well with morning and evening routines, but those seeking once‑daily convenience may look elsewhere.
Top Alternatives to Consider
Below are the most widely used alternatives, each with its own strengths.
Fluticasone Propionate
Fluticasone Propionate is a high‑potency inhaled corticosteroid marketed under brands like Flovent and Flovent Diskus, FDA‑approved in 1994. It can be effective at 100‑250µg once daily for many adults, thanks to its strong glucocorticoid receptor affinity. The drug’s lipophilicity leads to prolonged lung retention, which helps maintain symptom control with fewer doses. However, the higher potency may raise the risk of systemic effects such as cortisol suppression, especially at doses above 500µg daily.
Budesonide
Budesonide is a moderate‑potency inhaled steroid available as Pulmicort Turbohaler and Budesonide-formoterol combination (Symbicort), approved in 1992. Budesonide’s rapid oral absorption and high first‑pass metabolism keep systemic exposure low, making it a favorite for patients concerned about bone health or adrenal suppression. Typical dosing runs 200‑400µg twice daily, but the drug’s pleasant taste and easy‑to‑inhale design improve adherence for children.
Mometasone Furoate
Mometasone Furoate is a very high‑potency inhaled corticosteroid sold as Asmanex Twisthaler and Asmanex HFA, entering the market in 2005. Due to its strength, many patients achieve control with as little as 50‑100µg once daily. The convenience of a single daily inhalation is a major draw, though the potency can increase the likelihood of dysphonia and oral candidiasis if proper rinsing isn’t practiced.
Ciclesonide
Ciclesonide is a pro‑drug inhaled steroid that activates in the lungs, marketed as Alvesco, FDA‑approved in 2008. Because activation only occurs after inhalation, systemic exposure stays low even at higher inhaled doses. Doses of 80‑160µg once or twice daily are common. Users often report fewer instances of oral thrush, likely due to the drug’s low oropharyngeal deposition.
Side‑Effect Profile at a Glance
All inhaled steroids share a core set of local side effects, but the incidence varies with potency, particle size, and device type. Below is a concise matrix to help visualise the differences.
| Drug | Potency (relative to Beclomethasone) | Typical Daily Dose | Preferred Dosing Frequency | FDA Approval Year | Most Common Local Side Effects |
|---|---|---|---|---|---|
| Beclomethasone Dipropionate | 1× (reference) | 200‑800µg | Twice daily | 1975 | Oral thrush, hoarseness |
| Fluticasone Propionate | 1.5× | 100‑500µg | Once or twice daily | 1994 | Thrush, possible systemic cortisol suppression at high dose |
| Budesonide | 0.8× | 200‑800µg | Twice daily | 1992 | Thrush (lower incidence), mild systemic effects |
| Mometasone Furoate | 2× | 50‑200µg | Once daily | 2005 | Thrush, dysphonia |
| Ciclesonide | 1× (after activation) | 80‑320µg | Once or twice daily | 2008 | Lowest oral thrush rates, mild hoarseness |
How to Choose the Right Inhaled Steroid for You
Picking an inhaled corticosteroid isn’t just about potency; it’s about how the medication fits into daily life and health goals. Below are practical decision points you can run through with your prescriber.
- Dose frequency. If you struggle with twice‑daily routines, aim for a once‑daily option like Mometasone Furoate or a flexible once/twice schedule with Ciclesonide.
- Side‑effect tolerance. Patients with a history of oral thrush may benefit from Ciclesonide’s low oropharyngeal deposition.
- Systemic risk. For osteoporosis‑prone individuals, Budesonide’s rapid metabolism reduces systemic cortisol exposure.
- Device preference. Some people find metered‑dose inhalers (MDIs) easier than dry‑powder inhalers (DPIs). Beclomethasone and Fluticasone are available in both formats; Ciclesonide is only an MDI.
- Cost and insurance coverage. Generic Beclomethasone often has the lowest out‑of‑pocket price, while newer agents may require higher copays unless covered by a special formulary.

Real‑World Scenario Comparisons
Scenario 1 - A 28‑year‑old athlete with mild‑persistent asthma. The athlete wants a once‑daily regimen to avoid interrupting training. A low‑dose Mometasone Furoate (50µg once daily) provides sufficient control while keeping the pill burden low. Regular rinsing after use prevents throat irritation.
Scenario 2 - A 62‑year‑old with COPD and mild osteoporosis. Here, Budesonide’s favorable systemic profile is valuable. A twice‑daily 400µg dose maintains lung function without markedly affecting bone density, and the inhaler’s soft mist aids patients with limited inspiratory flow.
Scenario 3 - A 45‑year‑old with moderate asthma, heavy reliance on rescue inhaler. Switching from a low‑dose Beclomethasone to Fluticasone Propionate at 250µg once daily can tighten control, reduce rescue inhaler use, and potentially lower the risk of exacerbations that lead to ER visits.
Practical Tips for Maximising Benefits
- Always rinse your mouth with water and spit after each inhalation to cut down on thrush.
- Check your inhaler technique every few months; a poor seal can waste up to 30% of the medication.
- Use a spacer with MDIs if you have coordination challenges; it improves lung deposition.
- Schedule a follow‑up spirometry test after 4-6 weeks of any steroid change to confirm improved lung function.
- Keep a symptom diary; noting wheeze frequency, night-time awakenings, and rescue inhaler puffs helps your doctor fine‑tune the dose.
Frequently Asked Questions
Is Beclomethasone Dipropionate safe for long‑term use?
When used at the prescribed dose and combined with proper mouth‑rinsing, Beclomethasone Dipropionate is safe for many years. Monitoring bone density and eye pressure every 1-2 years is advisable for high‑dose users.
Can I switch from Beclomethasone to Fluticasone without a wash‑out period?
Yes. Both are inhaled steroids, so a direct switch is common. Your doctor will usually start you on an equivalent potency dose of Fluticasone and adjust based on symptom control.
Which inhaler has the lowest risk of oral thrush?
Ciclesonide, because it activates only after reaching the lungs, deposits less drug in the mouth and throat. Proper rinsing further reduces risk for any inhaled steroid.
Do inhaled steroids help with COPD as well as asthma?
Yes. Inhaled corticosteroids are a cornerstone of therapy for COPD patients with frequent exacerbations, especially when combined with long‑acting bronchodilators.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and continue with your regular schedule; don’t double‑dose.
Next Steps
If you’re ready to review your current inhaler, schedule an appointment with your respiratory therapist or primary care provider. Bring your medication list, note any side effects you’ve noticed, and discuss the dosing frequency that fits your daily routine. A quick spirometry test can confirm whether a switch to a higher‑potency, once‑daily steroid like Mometasone or Fluticasone could simplify your regimen without sacrificing control.
Remember, inhaled corticosteroids are most effective when paired with good inhaler technique, regular follow‑up, and an awareness of personal triggers. Whether you stick with Beclomethasone Dipropionate or move to an alternative, the goal stays the same: breathe easier and live fuller.




Craig Stephenson
October 6, 2025 AT 15:02Great overview! I appreciate the clear tables and the practical tips on rinsing after each puff. Makes it easier to pick the right inhaler for my routine.
Tyler Dean
October 8, 2025 AT 22:35All that pharma fluff hides the fact they’re pushing drugs to keep us hooked. Look at the side‑effect list – they’re marketing a problem.
Susan Rose
October 12, 2025 AT 09:55I love how the guide highlights cultural differences in inhaler preferences. Some folks prefer the sleek DPI, while others stick with the trusty MDI, and it’s good to see that respected.
diego suarez
October 14, 2025 AT 03:35Indeed, respecting device preference can improve adherence dramatically. When patients feel their choice is valued, they’re more likely to use the medication consistently, which ultimately leads to better control.
Eve Perron
October 17, 2025 AT 01:02What a wonderfully thorough exposition!; The author has meticulously charted each steroid’s potency, offering a clear hierarchy that even a layperson can grasp; Moreover, the inclusion of dosing frequencies alongside side‑effect profiles creates a multidimensional matrix that feels almost clinical in its precision; I particularly enjoy the way the guide doesn’t merely list data but weaves it into real‑world scenarios, such as the athlete needing a once‑daily regimen or the elderly COPD patient concerned about bone health; This narrative approach bridges the gap between raw numbers and lived experience, which is essential for shared decision‑making; The tables themselves are clean, well‑structured, and appropriately labeled, making quick reference a breeze; The author also makes a point of reminding readers about the critical act of rinsing after inhalation-a simple habit that can dramatically reduce oral thrush; It’s a detail that often gets lost in the blur of prescription instructions, yet here it is highlighted with deserved emphasis; Additionally, the discussion of pro‑drugs like ciclesonide underscores how pharmacology continues to evolve toward targeted activation, minimizing systemic exposure; The side‑effect matrix shows not only the frequency but also the severity, giving clinicians a nuanced view; I appreciate the balanced tone that neither demonizes nor glorifies any particular steroid, but instead focuses on patient‑centred outcomes; The guide’s “Next Steps” section encourages proactive dialogues with healthcare providers, a crucial component of chronic disease management; In short, this piece serves as both an educational primer and a practical toolkit, which is a rare combination in medical writing; Kudos to the author for delivering such a comprehensive resource with clarity and compassion; It truly empowers patients to take an active role in their respiratory health.
Josephine Bonaparte
October 18, 2025 AT 04:48Yo, that long paragraph was solid – clear, concise, and spot‑on!
Meghan Cardwell
October 19, 2025 AT 14:08From a pharmacodynamic perspective, the dose‑response curves of fluticasone versus budesonide illustrate a classic high‑affinity, low‑systemic‑exposure profile that translates into potent airway inflammation control with minimal adrenal impact; meanwhile, ciclesonide’s pro‑drug design leverages pulmonary esterases for on‑site activation, effectively reducing oropharyngeal deposition and thus curbing thrush incidence; the comparative potency ratios-2× for mometasone, 1.5× for fluticasone-guide clinicians toward the minimal effective dose principle, especially when balancing adherence convenience against systemic safety; in practice, selecting a once‑daily regimen can improve compliance, yet patient technique, device type, and inspiratory flow remain pivotal variables in achieving therapeutic success.
stephen henson
October 20, 2025 AT 12:22👍 Great breakdown, Meghan! The comparative PK really helps when counseling patients. 😊
Manno Colburn
October 21, 2025 AT 07:48so like i was thinkin about the whole inhaler ecosystem its kinda wild how pharma pushes these pro‑drugs like ciclesonide they say it’s safer but i wonder if the activation in lungs is really that perfect-i mean the enzyme variance among patients could lead to uneven activation which might cause patchy control… plus the cost factor sometimes forces patients to stick with older, less efficient options, and that can snowball into poor adherence, higher exacerbation rates, and ultimately more hospital visits; it’s a messy cycle that needs transparency and patient education to break.
Namrata Thakur
October 23, 2025 AT 01:28This guide shines a light on the importance of personalized inhaler selection. It encourages patients to discuss their lifestyle and concerns with their doctors, which is empowering.
Chloe Ingham
October 23, 2025 AT 15:22Dramatic but true – the right inhaler can change your life!