Why do patients keep taking expensive pills when cheaper, equally effective options are right there? It’s not about ignorance. It’s not about laziness. It’s about how our brains actually work - and that’s where behavioral economics comes in.
People Don’t Choose Drugs Like Robots
Traditional health policy assumes patients are rational actors. They see a $100 pill and a $30 pill that do the same thing? They pick the $30 one. Simple, right? But real life doesn’t work that way. A 2022 study found that 68% of patients stick with their current medication - even when a better-priced alternative exists. Why? Because switching feels risky. Even if the science says it’s safe, their brain says: What if something goes wrong? This isn’t stubbornness. It’s loss aversion. Behavioral economics shows we feel the pain of losing something twice as strongly as we feel the joy of gaining something equal. So giving up your familiar pill? That feels like a loss. Even if the new one is just as good.The Hidden Forces Behind Your Pill Decisions
Your choices about medication are shaped by invisible mental shortcuts - biases that even smart, informed people can’t escape.- Confirmation bias: You believe the more expensive drug must be better. A 2022 study showed prescription prices rose 47% faster than general inflation over the past decade - and patients still assume higher cost = higher quality.
- Present bias: You know you need to take your blood pressure pill every day, but right now? You’re fine. So you skip it. 33% of prescriptions are never even filled because the payoff feels too far away.
- Social norms: If you see other patients on a poster at the clinic taking their meds consistently, you’re more likely to do it too. One HIV study saw adherence jump 22.3% just by showing public adherence rates.
- Default options: When doctors’ electronic systems automatically suggest a certain drug, patients rarely change it - even if a cheaper option is available. One hospital increased appropriate drug substitutions by 37.8% just by changing the default setting.
How Much Does Non-Adherence Really Cost?
Skipping pills doesn’t just hurt your health - it breaks the system. In the U.S. alone, medication non-adherence leads to 125,000 preventable deaths every year and costs $289 billion in avoidable hospital visits, ER trips, and complications. That’s more than the entire annual budget of many U.S. states. And here’s the kicker: traditional patient education - pamphlets, videos, reminders - only improves adherence by 5-8%. Behavioral economics? It’s getting 14-28% improvements. One study gave patients a $10 rebate if they took their statin for 30 days straight. They stuck with it 23.8% longer than those who got no incentive. Why? Because losing $10 hurt more than gaining $10 felt good. That’s loss aversion at work.Why Nudges Work Better Than Lectures
Telling someone to take their medicine? That’s a lecture. Changing the environment so they take it without even thinking? That’s a nudge. A 2021 study tested two types of text reminders:- “Take your medication today.”
- “Don’t lose your streak!”
Who’s Doing This Right?
Big pharmaceutical companies aren’t waiting around. McKinsey found that firms using behavioral economics in patient support programs saw 17.3% higher medication persistence and 22.8% fewer discontinuations. Diabetes programs are leading the way. Why? Because daily insulin injections are visible, frequent, and tied to clear outcomes. It’s easy to track - and easy to nudge. Nearly half of all adherence programs now use behavioral tools. Meanwhile, oncology lags behind. Why? Because cancer treatments are brutal. Side effects are severe. Patients are overwhelmed. A nudge won’t fix that. Sometimes, the problem isn’t psychology - it’s pain.Barriers No Nudge Can Fix
Behavioral economics isn’t magic. It doesn’t work for everyone.- People with depression or anxiety see 31.4% less benefit from behavioral interventions.
- Patients on five or more medications have adherence rates 23.7% lower than those on one.
- Those with asymptomatic conditions - like high cholesterol or early-stage hypertension - are 32.7% less likely to stick with their meds because they don’t feel sick.
What’s Changing in Healthcare Policy
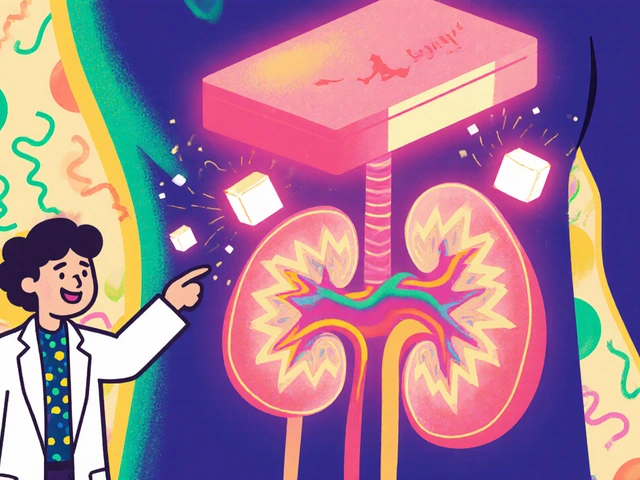
The FDA’s 2023 draft guidance now requires drug makers to evaluate how dosing frequency and pill size affect patient behavior. That’s huge. For the first time, regulators are forcing companies to think like behavioral economists. Medicare Part D now requires insurance plans to use at least two evidence-based behavioral interventions for high-risk patients. That means automatic refills, text reminders with loss-framing, and default substitutions are becoming standard. Pharmaceutical benefit managers (PBMs) - the middlemen who decide which drugs are covered - are now using behavioral insights to design formularies. Twenty-seven of the top 30 PBMs have added behavioral nudges into their drug selection rules.
Can This Work in Real Clinics?
Yes - but it’s not easy. Implementing these tools takes time. Clinics need 3-6 months to design, test, and train staff. Integration with electronic health records (EHRs) fails 78.3% of the time. And only 34.2% of programs keep their results after 12 months. Costs vary too. Smart pill bottles that track usage cost $47.50 per patient per month. Simple SMS reminders? $8.25. The cheaper option works - if it’s well-framed. And staff need training. Each clinician needs 12.7 hours to learn how to use these tools without overwhelming patients.The Future: Personalized Nudges
The next wave isn’t one-size-fits-all. It’s personalized. Researchers are now using machine learning to predict which patients will respond to which nudges. One pilot study showed that by analyzing age, income, medication history, and even social media habits, algorithms could predict who’d respond to loss-framed messages, who needed social pressure, and who just needed fewer pills. The result? A 42.3% boost in effectiveness. Imagine this: Your doctor gets an alert: “Patient X is likely to skip their blood thinner. Suggest a weekly pill pack + text reminder saying, ‘Your heart needs you - don’t break the chain.’” That’s not sci-fi. It’s happening now.What Patients Can Do
You don’t need a PhD to beat your own biases.- Ask: “Is this drug cheaper if I switch?” Don’t assume cost = quality.
- Request simpler regimens. Can you get a weekly pill instead of daily?
- Use apps that track your doses - and celebrate streaks.
- Be honest with your doctor about why you skip pills. Is it cost? Side effects? Fear? They can’t help if they don’t know.
What Providers and Pharmacies Can Do
Stop assuming patients are lazy or uninformed. Start designing systems that account for how humans really behave.- Make the healthy choice the easy choice. Default to generics unless the doctor opts out.
- Use loss-framed messaging: “You’ve taken 14 days in a row - don’t lose it.”
- Group patients by behavior type, not diagnosis. One-size-fits-all education fails.
- Track adherence not just by refill rates - but by real-time feedback.
Why do patients stick with expensive drugs even when cheaper ones are available?
Patients often stick with expensive drugs due to loss aversion - the fear of losing something familiar - and confirmation bias, where they believe higher cost equals better quality. Even when clinical evidence shows two drugs are equally effective, the emotional discomfort of switching outweighs the financial savings. Studies show 68% of patients won’t switch to a 30% cheaper alternative, even if it’s proven to work just as well.
What is a ‘nudge’ in behavioral economics?
A nudge is a subtle change in how choices are presented that guides people toward better decisions without restricting freedom. For example, making a generic drug the default option in a doctor’s electronic prescribing system - unless the doctor actively chooses otherwise - increases use of lower-cost alternatives by nearly 38%. Nudges work because they reduce mental effort and align with how people actually think, not how they should think.
Can behavioral economics improve medication adherence?
Yes - dramatically. While traditional education improves adherence by only 5-8%, behavioral interventions like loss-framed reminders, social norm feedback, and default options boost adherence by 14-28%. One study found patients given a rebate for consistent pill-taking stayed on their statins 23.8% longer. Text messages saying “Don’t lose your streak!” improved adherence by 19.7% compared to neutral reminders.
Are behavioral economics interventions ethical?
Yes - because they preserve choice. Unlike mandates or penalties, behavioral nudges don’t force anyone to act. A doctor can still override a default prescription. A patient can ignore a text reminder. Ethical concerns arise only when nudges are hidden or manipulative. Transparent, evidence-based nudges - like making generics the default - respect autonomy while making better outcomes easier to reach.
Why don’t all clinics use behavioral economics?
Implementation is complex. Integrating nudges into electronic health records fails 78% of the time. Staff need 12+ hours of training. Only 34% of programs maintain results after a year. Smaller clinics often lack funding or expertise - while academic centers have dedicated teams. Cost is also a barrier: smart pill bottles cost $47.50 per patient monthly, while basic SMS reminders cost $8.25. Many don’t know where to start.
Do behavioral interventions work for all conditions?
No. They work best for chronic conditions with clear, daily routines - like diabetes or hypertension. They struggle in areas like oncology, where side effects are severe and treatment is complex. Patients with depression or anxiety also respond 31% less effectively. Behavioral tools help when the barrier is psychology, not pain or scarcity.
What’s the future of behavioral economics in healthcare?
The future is personalization. Machine learning is being used to predict which patients respond to loss-framed messages, social pressure, or simplified dosing - based on their history, income, and behavior. Early trials show this boosts effectiveness by 42%. Digital therapeutics with real-time nudges are expected to grow 300% by 2026. Regulators like the FDA now require drug makers to consider patient behavior in design - meaning the next pill you take may be shaped by psychology, not just chemistry.





Marvin Gordon
December 5, 2025 AT 03:37Wow, this is one of those posts that makes you realize healthcare isn't broken-it's just designed for robots. I've seen friends skip meds because they 'felt fine,' and it's never about laziness. It's about how hard it is to care about tomorrow when today feels okay. Nudges aren't manipulation-they're just kindness with a blueprint.
Lucy Kavanagh
December 6, 2025 AT 12:05Of course the government and Big Pharma love this stuff-because now they can control what you take without you even knowing. Loss aversion? Please. They just want you hooked on $1200 pills and then slap a 'nudge' on it like it's magic. They don't care if you live-they care if you keep paying. This isn't science, it's psychological warfare dressed in lab coats.
Michael Dioso
December 7, 2025 AT 22:18Let me guess-next they’ll start putting little smiley faces on insulin pens to make you feel guilty for not taking it. 🤦♂️
Look, I get the theory. But 14-28% improvement? That’s not a revolution, that’s a Band-Aid on a hemorrhage. If your system relies on texting people ‘don’t lose your streak’ to keep them alive, you’ve already lost. The real fix? Lower prices. Not psychology hacks.
Krishan Patel
December 8, 2025 AT 18:14Behavioral economics is merely the modern veil over the ancient truth: man is not a rational creature, but a creature of habit, fear, and social mimicry. The pharmaceutical industry exploits this with surgical precision-not because they are evil, but because they are mirrors of our own irrationality.
We demand convenience, yet resent being guided. We crave autonomy, yet flee from responsibility. The $30 pill sits untouched while the $100 one is swallowed with reverence-not because it works better, but because we have been conditioned to equate price with virtue. This is not a flaw in the system-it is the system.
Deborah Jacobs
December 9, 2025 AT 07:01I used to skip my blood pressure meds until my sister sent me a sticky note that said: ‘Your heart remembers every time you forget.’ I cried. Then I started taking them. No app. No rebate. Just one dumbass note that made me feel seen.
People don’t need nudges-they need to feel like someone’s watching, and they matter. The science is cool, but the human part? That’s what sticks.
Stephanie Bodde
December 11, 2025 AT 00:46This is so true 😭 I had a friend who didn't take her statin for 8 months because she thought it 'made her tired'-turns out it was just her anxiety. Her doctor switched her to a weekly pill + a text that said 'You got this 💪' and boom-she’s been on it for a year. Small things. Huge difference. ❤️
Stephanie Fiero
December 12, 2025 AT 04:27so like… if i get a text saying ‘dont lose your streak’ but i dont even know what streak im on?? like wtf is this?? 🤷♀️ also why is my dr suddenly acting like my fitness coach??
Juliet Morgan
December 12, 2025 AT 10:09I work in a clinic and we tried the ‘don’t lose your streak’ texts. First week: 12% bump. Second week: 21%. Third week: 18%. We thought it was magic. Then we realized half the people didn’t even know they were in the program. The real win? When we started asking patients, ‘What’s stopping you?’-not telling them what to do. Turns out, most just wanted someone to listen.
Also, the $47 pill bottles? Waste of cash. The $8 texts? Perfect-if you actually know the person.
Chris Brown
December 14, 2025 AT 03:44Let me be the voice of reason in this sea of feel-good pseudoscience. You’re telling me that if we just rephrase a text message, people will suddenly take their pills? Where is the evidence that this doesn’t just delay the inevitable? People die because they can’t afford meds-not because they forgot to take them. This isn’t behavioral economics-it’s distraction economics. We’re polishing the coffin while ignoring the nail in the wall.
sean whitfield
December 14, 2025 AT 20:09So we’re paying billions to make people feel bad about skipping pills instead of making pills affordable? Brilliant. Next they’ll charge you extra if you don’t smile while taking your blood pressure med. At least the placebo effect was honest.
William Chin
December 15, 2025 AT 10:24As a physician who has spent 18 years watching patients self-sabotage their health, I can confirm: behavioral economics is not a fad-it is the only tool that has ever moved the needle in a measurable, sustainable way. The data is overwhelming. The resistance? It’s not about ethics-it’s about ego. Clinicians hate being told they’re not doing enough. Patients hate being told they’re irrational. But the truth? We’re all just flawed humans trying to survive. This isn’t manipulation. It’s medicine with humility.
Carole Nkosi
December 15, 2025 AT 17:10You want to know why this works? Because humans are not individual actors. We are echoes. We mirror. We follow. We fear being the outlier. That’s why showing public adherence rates works. It’s not about pills-it’s about belonging. The real tragedy? We treat mental health like a moral failure and then wonder why people don’t take their meds. We need to stop diagnosing behavior and start healing context.