Graves' disease is the most common cause of hyperthyroidism in the United States, affecting about 1 in 200 people. It’s not just an overactive thyroid-it’s an autoimmune war inside your body. Your immune system, which should protect you, mistakenly attacks your thyroid gland, tricking it into pumping out too much hormone. This leads to a cascade of symptoms: rapid heartbeat, weight loss, shaking hands, anxiety, and trouble sleeping. For many, it starts as "just stress"-until it doesn’t.
What Makes Graves’ Disease Different?
Not all hyperthyroidism is the same. In Graves’ disease, your body makes special antibodies called thyroid-stimulating immunoglobulins (TSI). These latch onto your thyroid like keys in a lock and force it to overproduce T3 and T4 hormones. That’s why blood tests show low TSH (below 0.4 mIU/L) and high free T4 (above 1.8 ng/dL) and free T3 (above 4.2 pg/mL). It’s a clear signal: your thyroid is running on overdrive.What sets Graves’ apart are the extra features. About half of people with this condition develop eye problems-bulging eyes, redness, double vision. This is called Graves’ ophthalmopathy. A smaller number get thickened, reddish skin on the shins or tops of feet, known as dermopathy. These aren’t side effects-they’re part of the disease itself. If you have bulging eyes and a fast heartbeat, Graves’ is the most likely culprit.
Why PTU? The Role of Propylthiouracil
When doctors need to calm down an overactive thyroid fast, they reach for antithyroid drugs. The two main ones are methimazole and propylthiouracil (PTU). Most adults start with methimazole-it’s easier to take (once a day), and it’s safer long-term. But PTU has a critical niche: early pregnancy.During the first trimester, methimazole carries a small but real risk of birth defects. PTU, while not perfect, is considered safer at this stage. That’s why it’s still used in pregnant women-even though it comes with a serious warning. The FDA requires a black box label on PTU because it can cause severe liver damage. About 1 in 500 people taking it develop liver injury, sometimes life-threatening. That’s why monthly blood tests for liver enzymes are mandatory. If you feel unusually tired, nauseous, or your skin turns yellow, stop the drug and call your doctor immediately.
PTU works by blocking the thyroid from making new hormones. It also stops the body from converting T4 into the more active T3. This dual action makes it faster at reducing symptoms in severe cases or thyroid storm-a medical emergency where your body overheats, your heart races over 140 beats per minute, and you can slip into coma. In those moments, PTU is often the first-line choice.
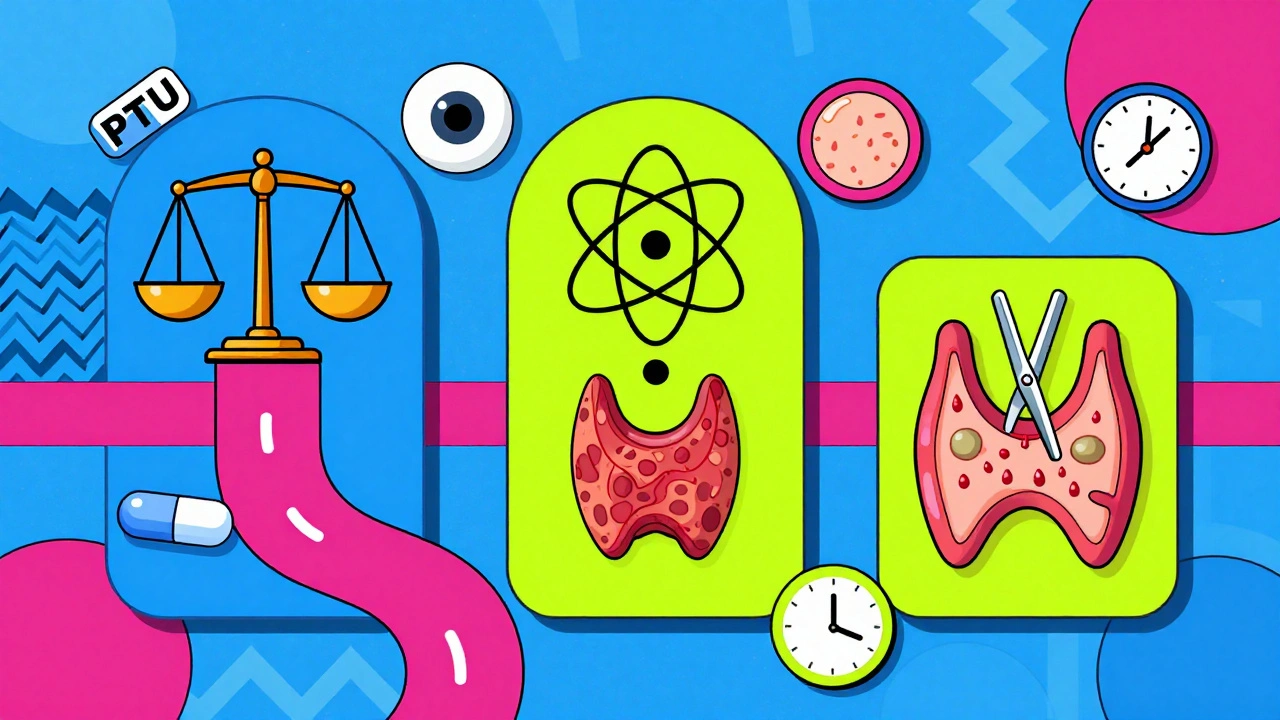
Treatment Options Compared
There are three main paths to treat Graves’ disease: drugs, radioactive iodine, or surgery. Each has trade-offs.
| Treatment | How It Works | Success Rate | Side Effects | Long-Term Outcome |
|---|---|---|---|---|
| PTU or Methimazole | Blocks hormone production | 70-80% control | Liver damage (PTU), skin rash, low white blood cells | 30-50% remission after 12-18 months; 40-60% relapse |
| Radioactive Iodine (I-131) | Destroys thyroid tissue | 80-90% | Permanent hypothyroidism, possible eye worsening | Requires lifelong thyroid hormone replacement |
| Thyroidectomy | Surgical removal of thyroid | 95% | Nerve damage, low calcium, voice changes | Permanent hypothyroidism; immediate symptom relief |
Radioactive iodine is the most common long-term fix in the U.S. It’s a pill you swallow. The radiation targets only your thyroid. Within months, your gland shuts down. You’ll need to take thyroid hormone for the rest of your life-but that’s usually simpler than managing fluctuating symptoms. Surgery is reserved for large goiters, pregnancy when drugs aren’t working, or if you can’t tolerate radiation.
Real-Life Challenges
Many people wait months before getting diagnosed. Symptoms like anxiety, weight loss, and insomnia are often blamed on stress, menopause, or burnout. One Reddit user shared they were told they had "generalized anxiety" for nine months before a blood test confirmed Graves’ disease. By then, they’d lost 18 pounds and couldn’t sleep through the night.
Even after treatment, problems don’t always disappear. About 40% of patients still have eye issues after their thyroid levels normalize. Some need steroid injections, orbital radiation, or even surgery to correct bulging eyes. And while PTU can save a pregnancy, the stress of monthly liver tests is real. One patient reported her ALT levels spiked to 120 U/L (normal is under 40) at 24 weeks. Her dose had to be cut in half.
Other side effects of PTU include a strange metallic taste, joint pain, and fatigue. Some people stop taking it because they feel worse on it than they did with the disease. That’s why close monitoring and open communication with your endocrinologist matter.
What Happens After Treatment?
Most people stay on antithyroid drugs for 12 to 18 months. Blood tests every 4 to 6 weeks check TSH and free T4 levels. If things stabilize, tests slow to every 2 to 3 months. After that, doctors try to wean you off. About one-third to half of people stay in remission. The rest relapse-often within a year of stopping the drug.
Testing for TRAb antibodies at diagnosis and again after treatment helps predict relapse. If your levels are above 10 IU/L after treatment, you have an 80% chance of the disease coming back. That’s a strong reason to consider radioactive iodine or surgery if you’re not planning pregnancy.
What’s New in Graves’ Disease?
The treatment landscape is changing. In 2021, the FDA approved teprotumumab, a drug that targets eye swelling in Graves’ ophthalmopathy. It’s not cheap-around $150,000 for a full course-but it reduces bulging eyes by 70% in most patients. It’s now an option for those who don’t respond to steroids.
Researchers are also testing drugs that block the TSH receptor directly. Early results show they can normalize thyroid function without causing hypothyroidism. That’s a game-changer. If it works long-term, it could mean treating Graves’ without destroying the thyroid or forcing lifelong hormone pills.
For now, PTU remains a vital tool-not because it’s ideal, but because it’s sometimes the only safe option for pregnant women. Its risks are real, but so are the risks of uncontrolled hyperthyroidism in pregnancy: premature birth, low birth weight, even fetal death.
When to Seek Help
If you have a racing heart, unexplained weight loss, trembling hands, or bulging eyes, get your thyroid checked. Don’t wait. Untreated Graves’ disease increases your risk of heart failure and atrial fibrillation by 20-30%. Thyroid storm, though rare, kills 20-30% of people who experience it.
Call your doctor right away if you have:
- Heart rate over 100 bpm at rest
- Fever above 100.4°F
- Severe nausea, vomiting, or confusion
- Yellow skin or dark urine (signs of liver damage)
- Sore throat or fever (possible agranulocytosis)
Support is out there. The Graves’ Disease and Thyroid Foundation offers a 24/7 helpline. Online communities like r/GravesDisease have over 12,000 members sharing tips, experiences, and reassurance. You’re not alone.
Final Thoughts
Graves’ disease isn’t a one-size-fits-all condition. Your treatment should match your life: your age, your plans for pregnancy, your tolerance for risk, and your symptoms. PTU isn’t the first choice for most-but for some, it’s the only choice that keeps both mother and baby safe. The goal isn’t just to lower hormone levels. It’s to restore your life.
With the right care, most people with Graves’ disease go on to live full, healthy lives. It takes patience, monitoring, and sometimes tough decisions. But recovery is possible.





dave nevogt
December 2, 2025 AT 19:49It’s funny how we reduce complex biological systems to binary choices-take the drug, or destroy the gland. But the body doesn’t care about convenience. It just wants balance. PTU isn’t a cure, it’s a ceasefire. And for pregnant women, it’s not even a choice-it’s a lifeline wrapped in risk. I’ve watched friends cycle through labs, anxiety, and guilt, all while trying to carry a life that depends on their own broken thyroid. The real tragedy isn’t the disease-it’s how little society acknowledges the invisible labor of managing chronic illness. Monthly blood draws, liver warnings, the metallic taste that never leaves your tongue… these aren’t side effects. They’re the cost of survival. And yet, we still treat it like a footnote in a medical textbook.
Maybe we need to stop seeing Graves’ as something to "fix" and start seeing it as something to live with-on your own terms, with your own rhythm, even if that rhythm includes a 120 U/L ALT spike at 24 weeks.
There’s no heroism in remission. Only quiet persistence.
And sometimes, that’s enough.
Ella van Rij
December 3, 2025 AT 12:25soo… PTU = liver death? lol. guess i’ll just let my thyroid melt my organs then. 🙃
also why is everyone so shocked that a drug with a black box warning has… a black box warning? like, did the FDA just slap a sticker on it and say ‘good luck lol’? 😭
also i think i have graves’ because i cried during a commercial for oat milk. not medically confirmed. just vibes.
Shannara Jenkins
December 5, 2025 AT 02:35Hey, I just wanted to say-reading this made me feel seen. I was misdiagnosed for 11 months too. Thought I was just ‘burnt out’ from grad school. Lost 20 lbs, couldn’t sleep, felt like my heart was trying to escape my chest. When the diagnosis finally came, I cried for an hour. Not because I was scared-I was relieved. Finally, something real.
PTU was brutal for me. Metallic taste? More like ‘licking a battery.’ But I stuck with it because I wanted to be a mom. My liver enzymes went up, my doc cut my dose, we monitored like hawks. I’m 32 weeks now. Baby’s kicking. I’m tired. But I’m here.
If you’re reading this and you’re on PTU? You’re doing better than you think. Even on the bad days. You’re not alone. I’ve got your back.
Elizabeth Grace
December 6, 2025 AT 12:24ok but like… why is everyone acting like PTU is some tragic hero drug? it’s literally a chemical grenade with a timer. i took it for 6 months and felt like a zombie with a bad taste in my mouth and joints that sounded like popcorn popping. and don’t even get me started on the monthly blood tests-like, i’m not a lab rat, i’m a person who just wants to nap without my heart doing the cha-cha.
also i’m pretty sure my dog started avoiding me because i smelled like a pharmacy. RIP, buttercup.
Joel Deang
December 8, 2025 AT 02:35bro i had graves’ and i was like ‘yo this is just stress’ for like 8 months then i passed out in the grocery store next to the organic kale. 😭
PTU? yeah i took it. tasted like regret and old pennies. liver tests every week like i was in the military. but i’m alive. baby’s alive. so i guess it worked? 🤷♂️
also if you’re on it and you feel weird? stop. don’t wait. just stop. your liver doesn’t care about your schedule.
ps: i still get weird eye dryness. like my eyeballs are in a desert. but hey, i got a 100k dollar eye drug now? that’s like… futuristic.
Jack Dao
December 8, 2025 AT 04:40It’s amusing how people treat Graves’ as if it’s a unique tragedy. The reality is that most autoimmune conditions are just poorly managed by a broken healthcare system. You take PTU? You’re gambling. You take radioactive iodine? You’re surrendering your biology to convenience. Surgery? You’re accepting permanent dependence. None of these are solutions-they’re compromises.
And yet, people still blame the patient for not ‘trying harder’ or ‘being more disciplined.’ If your thyroid is malfunctioning, it’s not because you ate too much gluten or didn’t meditate enough. It’s because your immune system is broken. And no amount of affirmations will fix that.
Also, teprotumumab at $150k? Of course. Because healthcare isn’t about healing-it’s about monetizing suffering. The real miracle isn’t the drug. It’s that anyone still believes in this system.
Steve World Shopping
December 10, 2025 AT 03:16From a global health systems perspective, the utilization of propylthiouracil in resource-constrained environments presents a significant risk-benefit asymmetry. While TSH-receptor antibody titers are diagnostic biomarkers, the absence of routine liver enzyme monitoring infrastructure in LMICs renders PTU pharmacovigilance nonviable. Consequently, the over-reliance on antithyroid drugs without adequate surveillance mechanisms contributes to iatrogenic hepatotoxicity cascades. Radioactive iodine, despite its immunological implications, remains the most cost-effective definitive modality in settings with functional nuclear medicine pipelines. The cultural fetishization of pharmacological ‘preservation’ of the thyroid gland is a high-income bias that disregards epidemiological pragmatism.
TL;DR: PTU is a Band-Aid on a hemorrhage-and only the privileged can afford to bleed slowly.
Jay Everett
December 11, 2025 AT 00:56Let me tell you something-Graves’ doesn’t care if you’re ‘strong’ or ‘positive.’ It doesn’t care if you’re a yoga instructor or a CEO. It just shows up like a party crasher who brings their own chaos.
PTU? Yeah, it’s messy. It’s scary. It makes your tongue feel like you licked a battery that was left in the rain. But here’s the thing-it’s the only thing standing between a pregnant woman and a fetal heart that’s beating too fast to survive.
I’ve seen patients go from ‘I can’t breathe’ to ‘I’m holding my baby’ on PTU. That’s not magic. That’s medicine doing its damn job, even when it’s ugly.
And yeah, the liver risks? Real. But so is the risk of untreated hyperthyroidism in pregnancy-preterm labor, preeclampsia, stillbirth. We don’t get to pick the cleanest path. We pick the path that lets someone live.
Also, teprotumumab? 150K? I know. It’s insane. But it’s also the first time in decades that we’ve had a treatment that actually *reverses* the eye damage. Not just masks it. Fixes it. That’s not just science-that’s hope with a price tag.
So yeah, PTU isn’t pretty. But sometimes, the most beautiful things in medicine are the ones that smell like regret and taste like pennies.
Keep going. You’re not broken. You’re just adapting.
🫂