Autoimmune hepatitis isn’t something you catch from someone else. It’s not caused by alcohol, viruses, or poor diet. It’s your own immune system turning against your liver-mistaking healthy liver cells for invaders and attacking them. Left untreated, this silent inflammation can lead to scarring, liver failure, or even the need for a transplant. But here’s the good news: with the right diagnosis and treatment, most people can stop the damage, reverse early scarring, and live normal, long lives.
How Is Autoimmune Hepatitis Diagnosed?
There’s no single test for autoimmune hepatitis. Doctors have to piece together clues from blood work, imaging, and a liver biopsy. That’s because symptoms are often vague-fatigue, joint pain, dark urine, or jaundice-things many people brush off as stress or the flu.
Blood tests are the first step. Elevated liver enzymes like ALT and AST are common, often five to ten times higher than normal. A key marker is immunoglobulin G (IgG), which tends to be significantly raised-usually more than 1.5 times the upper limit of normal. Autoantibodies like ANA (antinuclear antibodies) or SMA (smooth muscle antibodies) are also checked. In about 80% of cases, these are positive and point to Type 1 AIH, the most common form.
But here’s the catch: these antibodies aren’t perfect. Some people with AIH don’t have them. Others have them but don’t have the disease. That’s why a liver biopsy is still required. A small sample of liver tissue, taken with a thin needle under ultrasound guidance, shows the real damage. The hallmark sign is interface hepatitis-inflammation where the liver’s portal areas meet the surrounding tissue. Experts now say you need to see this pattern in at least 20 portal tracts to confirm the diagnosis.
Doctors use a scoring system called the Revised IAIHG criteria to put it all together. Points are given for antibody levels, IgG elevation, liver biopsy findings, and ruling out other causes like hepatitis B or C. A score above 15 means probable AIH. Above 20? That’s definite. This system keeps misdiagnoses low-especially important since AIH is rare, affecting only 10 to 25 people per 100,000.
Why Steroids Are the First Line of Treatment
Once autoimmune hepatitis is confirmed, treatment starts fast. The goal isn’t just to lower liver enzymes-it’s to shut down the immune attack before the liver turns to scar tissue. Corticosteroids, usually prednisone or prednisolone, are the fastest way to do that.
Within days, most patients start feeling better. Liver enzymes begin dropping. In fact, 80 to 90% of people show clear improvement within two weeks. That rapid response isn’t just a sign the treatment is working-it actually helps confirm the diagnosis. If your liver enzymes don’t drop after two weeks on steroids, your doctor will reconsider the diagnosis.
The standard starting dose is 0.5 to 1 mg per kilogram of body weight per day-up to a maximum of 60 mg daily. That’s a lot, and side effects show up fast. Weight gain, facial swelling (sometimes called "moon face"), mood swings, insomnia, and high blood sugar are common. About 70% of people on steroid-only treatment develop at least one major side effect within five years. That’s why doctors don’t keep you on high doses for long.
The plan is to taper the steroid slowly. By week 8, most patients are down to 10 to 15 mg per day. The goal is to get to the lowest possible dose that keeps the disease under control. But steroids alone aren’t the endgame. They’re just the beginning.
The Role of Azathioprine: Steroid-Sparing and Long-Term Control
Azathioprine (sold as Imuran or generic azathioprine) is the other half of the standard treatment. It’s an immunosuppressant that works differently than steroids. While steroids hit the brakes on inflammation quickly, azathioprine slowly reprograms the immune system to stop attacking the liver over time.
Its biggest advantage? It lets doctors cut steroid doses by 70 to 80% within six months. That means fewer side effects-less weight gain, less bone loss, fewer cataracts, and lower risk of diabetes. Studies show only 30% of patients on combination therapy develop serious steroid-related problems, compared to 70% on steroids alone.
The usual starting dose is 50 mg per day, then increased to 1 to 2 mg per kilogram of body weight-up to 150 mg daily. It’s taken daily, long-term. But it’s not without risks. About 1 in 10 people develop nausea, vomiting, or pancreatitis. A small number (about 12%) get bone marrow suppression, which lowers white blood cells and increases infection risk.
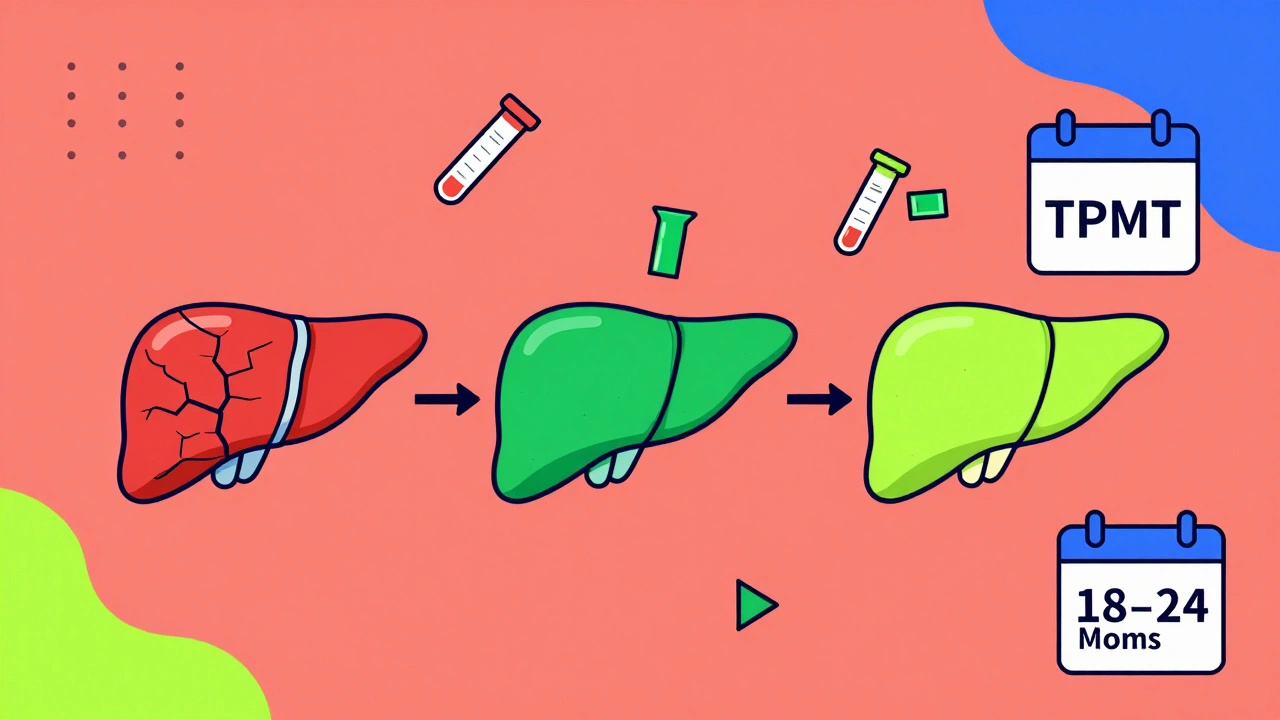
That’s why testing for TPMT enzyme levels is now standard before starting azathioprine. This enzyme breaks down the drug. People with very low or no TPMT activity (about 0.3% of the population) can develop life-threatening drops in blood cells if given normal doses. Testing costs $250 to $400 in the U.S., and while only 45% of U.S. centers do it routinely, nearly 80% of European centers do. It’s a simple blood test that can prevent serious harm.

How Long Do You Need to Stay on Treatment?
Many patients hope to stop treatment after a year or two. But here’s the hard truth: autoimmune hepatitis rarely goes away for good. About 60 to 80% of people need lifelong therapy to stay in remission.
Complete biochemical remission-normal liver enzymes and IgG levels-takes 18 to 24 months in 60 to 80% of patients. Histological remission, confirmed by a second biopsy showing no more interface hepatitis, happens in 50 to 70% after two to three years. That’s when doctors might consider trying to stop treatment.
But relapse is common. Between 50 and 90% of people who stop medication see the disease come back, often within three months. That’s why any attempt to stop treatment must be slow-tapering over six to twelve months-with monthly blood tests to catch early signs of flare-up. Only about 45% of people stay in remission two years after stopping.
For those who can’t tolerate steroids or azathioprine, second-line drugs like mycophenolate mofetil (CellCept) are used. About 25 to 30% of patients end up on these alternatives. Newer drugs like JAK inhibitors and anti-IL6 antibodies are showing promise in clinical trials, but they’re not yet standard.
What Happens If Treatment Fails?
Most people respond well. But 10 to 15% don’t improve after 12 to 18 months. That’s called treatment failure. It’s not the end-it just means the plan needs changing.
Doctors will first check if the patient is taking the medication correctly. Non-adherence is a bigger problem than people admit. Surveys show only 55% stick to steroid-only therapy, while 75% follow combination treatment. Missing doses can make drugs look ineffective when they’re not.
If adherence isn’t the issue, switching to mycophenolate or a calcineurin inhibitor like tacrolimus is the next step. In rare cases, liver transplantation becomes necessary. But that’s only needed in about 5% of patients, usually those who’ve already developed cirrhosis or liver failure.
What You Can Do to Protect Your Liver
Medication is key-but your daily choices matter too. Avoid alcohol completely. It adds extra stress to an already inflamed liver. Get vaccinated for hepatitis A and B before starting immunosuppressants. Once you’re on steroids or azathioprine, your immune system won’t respond well to vaccines. If you haven’t been vaccinated yet, you might not be protected.
Test for hepatitis B before starting treatment. About 15 to 20% of people carry the virus silently. Immunosuppressants can wake it up, causing a dangerous flare. If you test positive, you’ll need antiviral drugs like tenofovir alongside your AIH treatment.
Watch your bone health. Steroids weaken bones. Take calcium and vitamin D. Ask your doctor about a bone density scan if you’ve been on steroids longer than six months. Stay active. Walking, swimming, or light resistance training helps keep bones strong and manage weight gain.
And don’t ignore mental health. Mood swings, anxiety, and depression are common with steroids. Talk to your doctor. Support groups like the American Liver Foundation or Reddit’s r/liverdisease community can help you feel less alone.
What’s New in 2025?
The latest guidelines from the European Association for the Study of the Liver (EASL), released in January 2025, made big changes. They no longer recommend splitting AIH into Type 1 and Type 2 based on autoantibodies. Why? Because it doesn’t change how you treat it. Whether you have ANA or LKM1, you still get steroids and azathioprine.
Another shift: doctors now wait 6 to 12 months to judge treatment response, not just 6 months. Some people take longer to respond. Rushing to change treatment too soon can lead to unnecessary switches.
There’s also new hope on the horizon. Obeticholic acid (Ocaliva), originally used for another liver disease, is now in Phase 3 trials for AIH. Early results show a 42% complete response rate-better than standard therapy. And researchers are testing blood tests that can predict who will respond to steroids within two weeks, using microRNA markers. That could mean personalized treatment plans in the near future.
For now, the basics still hold: diagnose early, treat with steroids and azathioprine, monitor closely, and never stop treatment without medical guidance. The disease is chronic-but it’s manageable. Thousands of people are living full lives with it, thanks to these proven treatments.
Can autoimmune hepatitis be cured?
Autoimmune hepatitis can’t be cured in the traditional sense. The immune system doesn’t suddenly stop attacking the liver. But with treatment, most people achieve long-term remission-meaning the disease is under control, liver damage stops, and sometimes even reverses. Many live normal lives on low-dose medication. Stopping treatment usually leads to relapse, so lifelong management is often needed.
How long does it take for azathioprine to work?
Azathioprine doesn’t work quickly. While steroids reduce liver enzymes in days, azathioprine takes 3 to 6 months to show full effect. That’s why it’s used alongside steroids at first. The goal isn’t immediate relief-it’s long-term immune control. You’ll need to be patient. Blood tests every few weeks will track progress.
Can I drink alcohol with autoimmune hepatitis?
No. Alcohol puts extra stress on your liver, which is already under attack. Even small amounts can speed up scarring and reduce the effectiveness of your medications. Complete abstinence is the only safe choice. This isn’t a suggestion-it’s a medical necessity.
What are the most common side effects of steroids?
The most common side effects include weight gain (especially around the face and abdomen), mood swings, trouble sleeping, increased appetite, high blood sugar, and bone thinning. Some people develop cataracts or high blood pressure. These are dose-dependent, so tapering the steroid slowly helps reduce them. Most side effects improve once the dose is lowered.
Is azathioprine safe for long-term use?
Yes, for most people. Azathioprine has been used safely for decades in autoimmune diseases. The biggest risks are bone marrow suppression and pancreatitis, which are rare. Regular blood tests every 3 months check your white blood cell count and liver function. TPMT testing before starting helps avoid the most serious risks. If you’re monitored properly, long-term use is standard and safe.
Can I get pregnant while on azathioprine or steroids?
Yes, many women with autoimmune hepatitis have healthy pregnancies while on low-dose steroids and azathioprine. In fact, staying on treatment during pregnancy is safer than stopping it, because a flare can harm both mother and baby. Talk to your hepatologist and OB-GYN before trying to conceive. Doses may be adjusted, but stopping medication increases the risk of liver damage during pregnancy.
How often do I need blood tests?
During the first few months of treatment, you’ll need blood tests every 2 to 4 weeks to monitor liver enzymes and blood counts. Once stable, every 3 months is typical. IgG levels are checked quarterly. If you’re on azathioprine, your white blood cell count is tracked closely. Any sudden rise in ALT or AST could mean a flare-don’t wait for your next appointment if you feel worse.
Do I need a liver biopsy every year?
No. A second biopsy is usually done after 18 to 24 months of treatment to check for histological remission. After that, biopsies aren’t routine unless your blood tests suggest a flare or your doctor suspects disease progression. Most monitoring is done with blood tests and clinical symptoms.






Chase Brittingham
December 4, 2025 AT 09:44Just wanted to say thanks for laying this out so clearly. I was diagnosed last year and this is the first time I’ve read something that didn’t feel like a textbook. The part about TPMT testing saved me-I had no idea it was even a thing until my doctor mentioned it. Still on low-dose steroids and azathioprine, and honestly? I feel better than I have in years.
Joe Lam
December 5, 2025 AT 18:34Of course you feel better-you’re on immunosuppressants. The real question is whether you’re just delaying the inevitable. The liver doesn’t regenerate forever, and these drugs are basically chemical brute force. Anyone who thinks this is ‘manageable’ is ignoring the fact that we’re just patching a sinking ship with duct tape and hope.
Jenny Rogers
December 6, 2025 AT 06:16While I appreciate the clinical precision of the post, I must emphasize the ethical imperative of recognizing autoimmune hepatitis not merely as a biochemical aberration, but as a profound metaphysical disruption of the body’s innate harmony. The immune system does not ‘mistake’ hepatocytes-it is responding to a deeper systemic dissonance, likely rooted in chronic stress, environmental toxins, or spiritual neglect. Pharmacological suppression, while expedient, fails to address the ontological root.
Rachel Bonaparte
December 7, 2025 AT 20:37Okay but have you heard about the 2024 CDC whistleblower report? They buried data showing that azathioprine was linked to a 300% spike in rare lymphomas in patients under 40-only the pharma lobby kept it quiet. And don’t get me started on the ‘steroid taper’-it’s all a scam to keep you hooked. I’ve been off meds for 18 months now, just did a 14-day juice cleanse and my liver enzymes are NORMAL. The real enemy isn’t your immune system-it’s Big Pharma pushing toxic chemicals to keep you dependent. TPMT testing? That’s just another way to monetize your fear. I’m not saying this to scare you-I’m saying this to wake you up.
Scott van Haastrecht
December 9, 2025 AT 07:57Let’s be brutally honest: 80% of people on this thread are just looking for validation that they’re not dying. You think your ‘remission’ means anything? Your enzymes are normal because you’re chemically sedated. The moment you stop, the inflammation comes back with a vengeance. And the biopsy? A $5,000 gamble. Most doctors don’t even know how to interpret portal tract counts correctly. This isn’t medicine-it’s a confidence game with a lab report.
Bill Wolfe
December 9, 2025 AT 08:12😂😂😂 I love how everyone acts like they’re the first person to ever have this. You think you’re special because you got diagnosed? I’ve been on azathioprine since 2012. My IgG levels are still elevated, my liver’s got more scars than a biker’s arm, and I still have moon face. But hey-at least I’m alive. And yes, I did get my TPMT tested. And no, I didn’t cry when I saw the results. 🤷♂️
Ollie Newland
December 11, 2025 AT 07:23From a hepatology perspective, the EASL 2025 update is a watershed moment-particularly the de-emphasis on serotype stratification. The data clearly shows no differential response to first-line therapy between ANA+ and LKM1+ cohorts. That said, the 6–12 month response window is clinically sound; early switch decisions based on incomplete biochemical normalization are a leading cause of therapeutic nihilism. Also, obeticholic acid’s phase 3 data is promising-though I’d caution against overextrapolating from ALT normalization alone without histological correlation.
Rebecca Braatz
December 12, 2025 AT 01:56YOU GOT THIS. I know it feels overwhelming right now, but you’re not alone. I was diagnosed at 28, thought my life was over, and now I’m hiking mountains and teaching yoga. Yes, the meds suck. Yes, the blood tests are annoying. But you’re fighting for your future-and that’s something to be proud of. Find your tribe. Talk to someone. You’re stronger than you think. 💪❤️
Michael Feldstein
December 12, 2025 AT 11:56What’s the longest someone’s stayed in remission after stopping meds? I’ve heard 45% stay in remission two years out, but has anyone gone 5+ years? I’m asking because my mom’s been off everything for seven years now and her liver’s fine-no biopsy since 2017. Just curious if that’s a fluke or if there’s a pattern.
Chase Brittingham
December 13, 2025 AT 14:07That’s actually not a fluke. I know a guy who stopped at 8 years-had a biopsy, everything looked clean. But he was meticulous: no alcohol, no NSAIDs, strict sleep schedule, and he did monthly labs. Most people who relapse stop monitoring. It’s not about being cured-it’s about being disciplined.
Kathleen Koopman
December 14, 2025 AT 18:59Wait… so if I’m on azathioprine, can I still get the shingles vaccine? 🤔
Melania Dellavega
December 15, 2025 AT 04:41There’s a quiet dignity in living with this. Not the dramatic ‘I beat it’ narrative, but the daily quiet choice to show up-to take the pill, to get the bloodwork, to say no to the drink, to sit with the fear and still breathe. We don’t need to be heroes. We just need to be consistent. The liver doesn’t care about your Instagram posts. It only cares if you show up for it, day after day.
Precious Angel
December 15, 2025 AT 05:20They told me I needed steroids. I refused. I went to a naturopath. She gave me turmeric, milk thistle, and a 30-day ‘liver detox’ with lemon water and ‘energy healing.’ Six months later, my ALT was 1,200. They had to put me in the hospital. Now I’m on azathioprine. I don’t hate them-I hate the people who told me ‘natural’ was better. This isn’t a lifestyle blog. This is your liver screaming for help. Stop listening to influencers. Listen to your doctor.
Melania Dellavega
December 15, 2025 AT 11:43That’s why I never say ‘you should’ve listened.’ I say ‘you’re still here.’ And that matters more than any protocol. You survived the crash. Now you’re learning how to fly with the wings you’ve got.