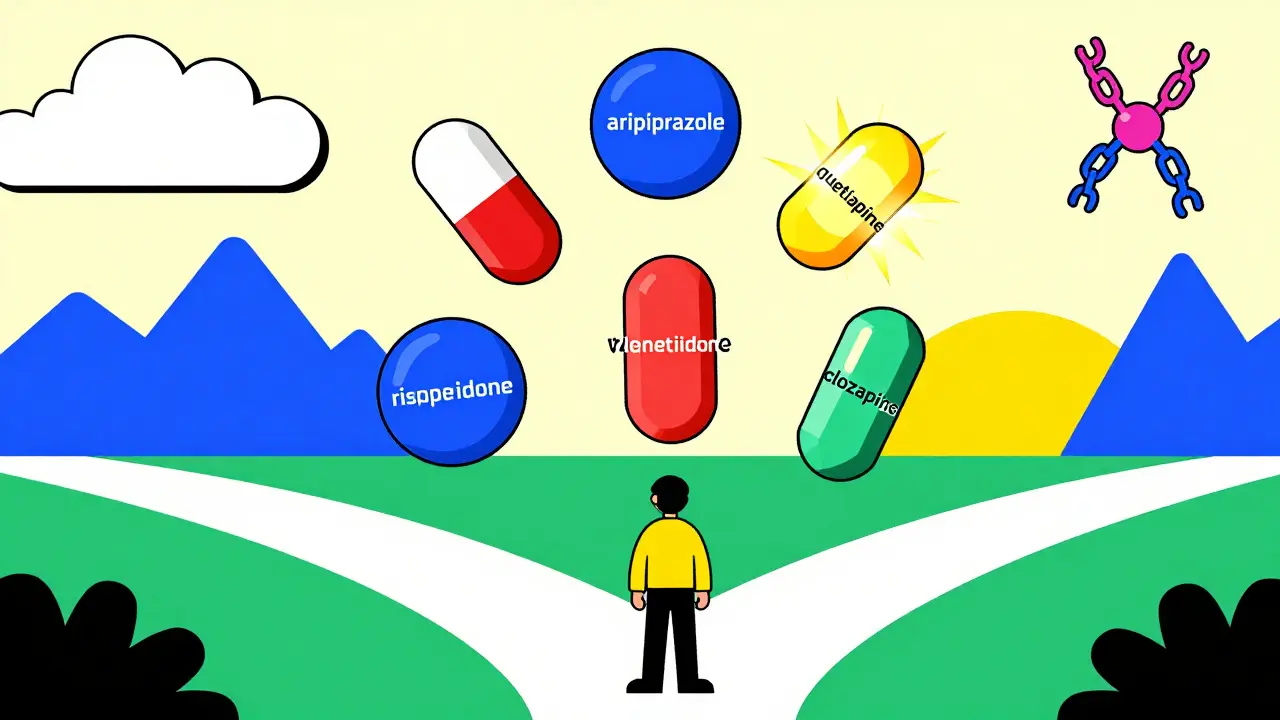
When someone is diagnosed with schizophrenia, the road to stability often begins with medication. But not all antipsychotics are the same. The choice isn’t just about stopping hallucinations or quieting delusions-it’s about finding a balance between symptom control and daily life. For many, the first pill prescribed doesn’t work. Or it causes weight gain so severe they can’t keep taking it. Or it makes their hands shake so badly they avoid going out. This isn’t rare. It’s the norm. And understanding the difference between first-generation and second-generation antipsychotics can change everything.
What Are Antipsychotics, Really?
Antipsychotic medications are the backbone of schizophrenia treatment. They don’t cure the illness, but they help manage the most disruptive symptoms: hearing voices, feeling watched, believing things that aren’t true. About 0.5% of people worldwide live with schizophrenia, and for most, medication is essential. The two main types are first-generation (FGAs) and second-generation (SGAs), sometimes called atypical antipsychotics.
First-gen drugs like haloperidol and chlorpromazine came out in the 1950s. They work by blocking dopamine, a brain chemical linked to psychosis. But they also block dopamine in areas that control movement. That’s why up to half of people on these drugs develop tremors, stiffness, or restlessness-side effects called extrapyramidal symptoms. These can be so uncomfortable that many stop taking the meds, even if they’re helping.
Second-gen drugs, developed starting in the 1980s, were meant to fix that. They still block dopamine, but they also affect serotonin, another brain chemical. This shift made them less likely to cause movement problems. But they came with new trade-offs: weight gain, high blood sugar, and increased risk of diabetes. The most commonly prescribed today include aripiprazole, olanzapine, quetiapine, and risperidone.
Why Atypical Antipsychotics Are First-Line
Current guidelines from the American Psychiatric Association recommend second-generation antipsychotics as the first choice for most people with schizophrenia. Why? Because they’re better tolerated. A 2023 study tracking nearly 28,500 patients found that those on aripiprazole had a 18.2% chance of relapse within a year, compared to 29.7% for those on haloperidol. That’s a big difference. But it’s not just about effectiveness-it’s about sticking with the treatment.
Studies show that 63% of people stop their first antipsychotic within six months. The reasons? Sedation, weight gain, or movement issues. Olanzapine, for example, is powerful at controlling symptoms, but 78% of users on Reddit reported major weight gain. Quetiapine causes drowsiness so intense that some can’t hold down jobs. Risperidone can cause breast enlargement or loss of libido. These aren’t rare side effects. They’re expected.
That’s why doctors now start with SGAs-not because they’re perfect, but because they give people a better shot at staying on treatment. And staying on treatment means fewer hospitalizations, fewer crises, and more stability.
Clozapine: The Last Resort That Works
When two or more antipsychotics fail, there’s still one option: clozapine. It’s not used first because it’s dangerous. It can wipe out white blood cells, leaving the body vulnerable to infection. That’s why anyone on clozapine needs weekly blood tests for the first six months. It’s a hassle. It’s expensive. But for those with treatment-resistant schizophrenia, it’s life-changing.
A 10-year study of over 17,000 patients found clozapine kept people on medication longer than any other drug-over 500 days on average. In one case, a patient who’d tried five medications said, “Clozapine gave me my life back despite the blood tests.” That’s not hyperbole. Studies show clozapine reduces treatment resistance by 30-50%. But only 1 in 4 people with treatment-resistant schizophrenia in the U.S. get it. In Finland, it’s 40%. Why the difference? Access. Cost. Fear of side effects.
The Clozapine REMS program in the U.S. was created to make monitoring safer. It reduced discontinuations by 18%, but it also created barriers-especially in rural areas where clinics don’t have the staff to manage the paperwork. For many, the system itself becomes part of the problem.
How Do These Drugs Compare?
There’s a myth that all antipsychotics work the same. They don’t. Here’s how some key drugs stack up based on real-world data:
| Medication | Typical Daily Dose | Relapse Risk (12 Months) | Average Weight Gain | Movement Side Effects |
|---|---|---|---|---|
| Aripiprazole | 10-15 mg | 18.2% | 0.6 kg | 4.1% |
| Paliperidone | 6-12 mg | 20.5% | 1.7 kg | 7.3% |
| Olanzapine | 10-20 mg | 26.8% | 4.2 kg | 9.7% |
| Quetiapine | 400-800 mg | 28.1% | 2.8 kg | 6.2% |
| Risperidone | 2-8 mg | 27.4% | 1.9 kg | 18.3% |
| Clozapine | 300-600 mg | 15.3% | 4.5 kg | 1.8% |
| Haloperidol | 5-20 mg | 29.7% | 0.9 kg | 35% |
Notice something? Aripiprazole has the lowest weight gain and lowest movement side effects. But it’s not the most effective for everyone. Paliperidone, a longer-acting version of risperidone, has lower relapse rates than oral risperidone. And clozapine, despite its risks, has the lowest relapse rate of all.
Long-Acting Injections: A Game-Changer
Many people stop taking pills because they forget, or because they don’t feel like taking them every day. That’s where long-acting injectables (LAIs) come in. These are shots given every 2 to 4 weeks that release medication slowly. They’re not new, but their use is growing fast.
In Europe, 30% of antipsychotic prescriptions are LAIs. In the U.S., it’s 25%. Paliperidone palmitate, given once a month, reduces discontinuation by 22% compared to oral risperidone. For someone who’s been hospitalized multiple times, this isn’t just convenient-it’s life-saving.
But access is uneven. Many clinics don’t offer LAIs. Insurance doesn’t always cover them. And some patients fear needles. Still, for those who struggle with adherence, LAIs can be the difference between stability and crisis.
The Real Cost: Side Effects and Quality of Life
Medication isn’t just about symptoms. It’s about how you feel every day. One man on Reddit wrote: “Aripiprazole helped my voices, but the restlessness made me pace all night. I couldn’t sleep. I quit.” That’s akathisia-a common side effect of aripiprazole. It’s not just discomfort. It’s torture.
Weight gain is another silent crisis. Olanzapine and clozapine can add 4-5 kilograms in the first year. That leads to diabetes, heart disease, low self-esteem. And it’s not just about eating more. These drugs change how your body processes sugar and fat. Metformin, a diabetes drug, can cut weight gain by 4.2 kg in six months. But few doctors offer it as a preventive measure.
And then there’s the emotional toll. One woman said, “I feel like I’m in a fog. I can’t think clearly. I don’t care about anything.” That’s not psychosis. That’s sedation. And it’s common with quetiapine and olanzapine.
What’s Next? New Hope on the Horizon
Science isn’t standing still. In 2023, the FDA approved lumateperone for schizophrenia with bipolar depression. It works differently-targeting serotonin and dopamine without the weight gain. In trials, it improved symptoms without the metabolic risks of older drugs.
Even more promising are drugs like KarXT and SEP-363856. KarXT, a new type of medication that acts on muscarinic receptors, showed a 9.6-point drop in symptom scores-far better than placebo. SEP-363856, a TAAR1 agonist, cut symptoms without causing weight gain. And ALKS 3831 combines olanzapine with a drug that blocks appetite, reducing weight gain by 63%.
But these aren’t magic bullets. None of them fix negative symptoms-like lack of motivation or emotional flatness. And they’re still years away from widespread use.
Choosing the Right Medication
There’s no one-size-fits-all. The best drug is the one you can take without losing your life to side effects. Here’s how to think about it:
- If you’re young and active, and weight gain is a big concern: start with aripiprazole or ziprasidone.
- If sleep is a problem and you need strong symptom control: quetiapine might help-but prepare for drowsiness.
- If you’ve tried two or more drugs and still have symptoms: ask about clozapine. The blood tests are a burden, but the results can be life-changing.
- If you forget pills: ask about a long-acting injection like paliperidone palmitate.
- If you have diabetes or high cholesterol: avoid olanzapine and clozapine unless absolutely necessary.
And always-always-talk to your doctor about side effects. Don’t wait until you quit. Don’t hide how you feel. There are ways to manage them. Metformin. Exercise. Dose changes. Switching drugs. You’re not stuck with the first pill you’re given.
Final Thoughts
Schizophrenia treatment isn’t about finding the perfect drug. It’s about finding the right one for you. Some people thrive on aripiprazole. Others need clozapine. Some do better with a shot every month. The goal isn’t to be symptom-free-it’s to be able to live. To work. To connect. To sleep through the night without shaking. To feel like yourself again.
The science is clear: antipsychotics work. But they’re not all the same. And your experience matters more than any guideline. If one drug doesn’t work, it doesn’t mean you’re broken. It just means you haven’t found the right one yet.




Daniel Dover
February 16, 2026 AT 06:16Virginia Kimball
February 17, 2026 AT 16:06Charlotte Dacre
February 19, 2026 AT 10:32Mike Hammer
February 20, 2026 AT 04:42Chiruvella Pardha Krishna
February 20, 2026 AT 09:42Mandeep Singh
February 20, 2026 AT 23:33Josiah Demara
February 22, 2026 AT 11:34Kaye Alcaraz
February 24, 2026 AT 05:12Sarah Barrett
February 24, 2026 AT 21:27Erica Banatao Darilag
February 24, 2026 AT 22:53Esha Pathak
February 26, 2026 AT 16:57Kapil Verma
February 27, 2026 AT 20:53