Imagine looking at a street sign, but the letters keep blurring and doubling. You squint. You lean forward. You rub your eyes. Nothing helps. This isn’t just bad eyesight. It’s keratoconus-a slow, silent change in the shape of your cornea that turns clear vision into a constant struggle. It doesn’t happen overnight. It creeps in during your teens or twenties, often starting in one eye before the other. And while glasses won’t fix it, there’s a solution that’s helped millions: rigid contact lenses.
What Actually Happens in Keratoconus?
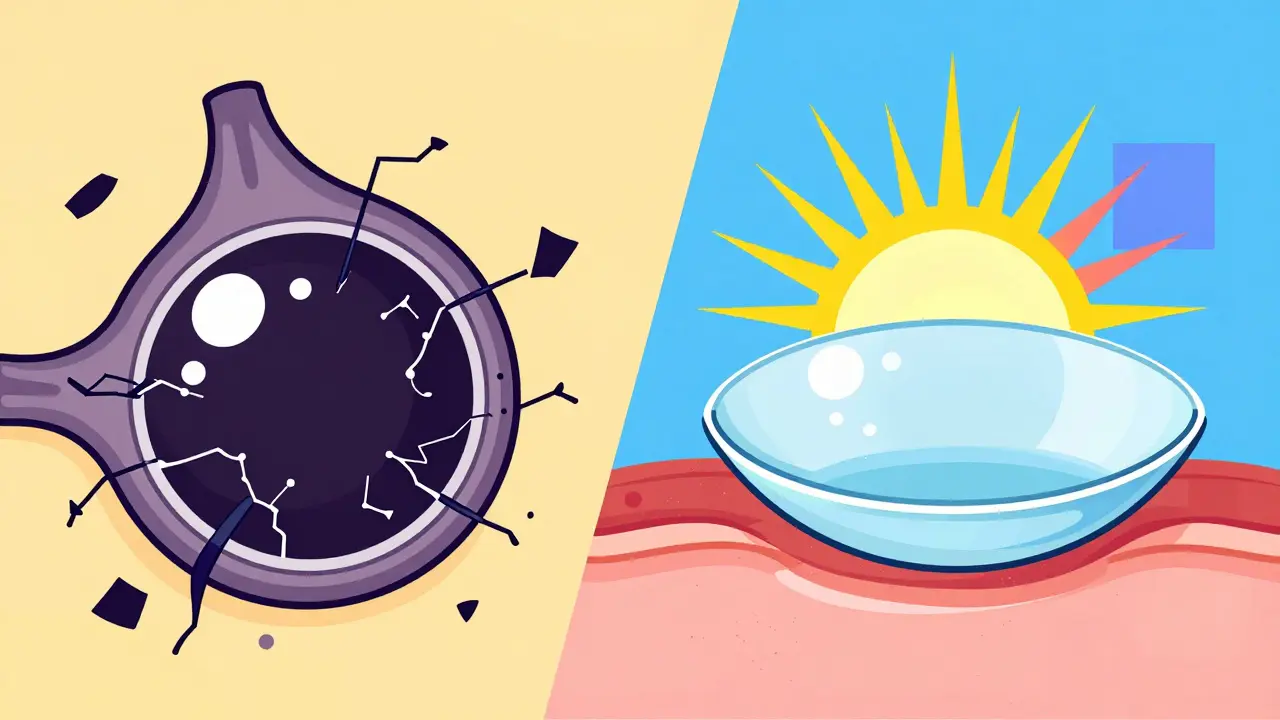
Your cornea is the clear, dome-shaped front surface of your eye. It’s not just a window-it’s the first lens your eye uses to focus light. In keratoconus, this structure weakens. The collagen fibers that hold it in place start breaking down. Enzymes chew through the tissue, and the body doesn’t make enough to stop it. The result? The center of the cornea slowly bulges outward into a cone shape. This isn’t just cosmetic. That cone distorts how light enters your eye. You get blurry vision, ghost images, glare at night, and sudden changes in your prescription. Most people think they just need stronger glasses. But glasses can’t fix an irregular surface. They’re designed for smooth curves. When the cornea is warped, glasses just make the blur worse. Keratoconus usually stops progressing by your 40s. But until then, it can get bad fast. About 1 in 2,000 people have it. It’s not rare. And it’s not just a problem for teens-it shows up in adults too, often missed because symptoms are blamed on eye strain or aging.Why Rigid Lenses Work When Glasses Don’t
Soft contact lenses are flexible. They mold to your cornea. That’s great for normal eyes. But when your cornea is cone-shaped, a soft lens just follows the curve-trapping the distortion instead of fixing it. Rigid lenses are different. They’re stiff. They don’t bend. When you put one on, it floats just above your cornea, creating a smooth, perfectly round optical surface. Think of it like putting a clear, hard plastic dome over a crumpled piece of paper. The paper is still wrinkled underneath, but the surface you see is flat. That’s what rigid lenses do for your vision. Studies show patients go from seeing 20/400 (legally blind) to 20/200 or better after fitting. Some reach 20/25. That’s not magic. It’s physics. The rigid lens replaces the irregular cornea with a perfect refractive surface. There are three main types:- RGP lenses: Small, hard lenses (9-10mm) made from oxygen-permeable materials. Dk values range from 50 to 150, meaning your cornea still gets enough oxygen to stay healthy.
- Hybrid lenses: A rigid center for clarity, surrounded by a soft ring for comfort. Good for people who find RGP lenses too uncomfortable.
- Scleral lenses: Larger (15-22mm), vaulting over the entire cornea and landing on the white of the eye (sclera). They create a fluid reservoir between the lens and cornea, cushioning the irregular surface. This is the go-to for advanced cases.
How Scleral Lenses Changed the Game
Ten years ago, people with severe keratoconus had two choices: suffer with poor vision or get a corneal transplant. Now, scleral lenses are the first-line treatment for stage III and IV keratoconus. Why? Because they don’t touch the damaged part of the cornea at all. The lens sits on the sclera, and the space between it and the cornea fills with saline. That fluid acts like a liquid bandage-smoothing out the cone, reducing irritation, and even helping the cornea heal slightly over time. Studies show scleral lenses work in 85% of advanced cases, compared to 65% for traditional RGP lenses. They’re also more comfortable. People who couldn’t wear any lens for years now wear them all day. One patient in Perth told me she hadn’t driven at night for seven years. After her first scleral lens fitting, she drove to the beach. Just because she could see the headlights clearly. New materials now have oxygen permeability over Dk 200-better than most soft lenses. And since January 2023, the FDA has approved digital manufacturing for fully customized scleral lenses. Each one is built from a 3D scan of your eye. No more trial-and-error fittings.
What About Corneal Cross-Linking?
Rigid lenses fix your vision. But they don’t stop the cornea from getting worse. That’s where corneal cross-linking (CXL) comes in. CXL is the only treatment proven to halt keratoconus progression. It uses UV light and riboflavin (vitamin B2) to strengthen the collagen bonds in your cornea. Think of it like adding superglue to the structure. The FDA approved it in 2016. Success rates? 90-95% over five years. Here’s the catch: CXL doesn’t improve your vision. It just stops it from getting worse. So most people need both. CXL first, then rigid lenses to restore sight. About 78% of cornea specialists now recommend this combo. It’s not optional anymore-it’s standard.Other Options-and Why They’re Not Always Better
Some people hear about INTACS or transplants and think those are better. But they’re not. INTACS are tiny plastic rings inserted into the cornea to flatten the cone. They help a bit. But 35-40% of people still need rigid lenses after the procedure. It’s not a replacement-it’s a supplement. Corneal transplants? They’re a last resort. Only 10-20% of keratoconus patients ever need one. Why? Because transplants carry risks: rejection (5-10%), infection, and vision that takes over a year to stabilize. Even after a successful transplant, many still need rigid lenses for sharp vision. Rigid lenses are non-invasive. Reversible. Adjustable. And they work for most people. That’s why 60-70% of diagnosed patients use them as their main treatment.The Fitting Process: What to Expect
Getting rigid lenses isn’t like buying glasses. It’s a process. First, your eye doctor will map your cornea with a topographer-a machine that creates a 3D map of its shape. This tells them exactly where the cone is and how steep it is. Then comes the trial. You’ll try several lens designs over 3-5 visits. Each one is adjusted: diameter, curve, thickness, edge design. It can take 4-6 weeks to get it right. Once fitted, you start slow. Wear them 2-4 hours a day. Add an hour every couple of days. Most people reach full-time wear in 2-4 weeks. You’ll learn:- How to insert and remove them without touching your cornea
- How to clean them daily with prescribed solutions
- How to spot warning signs: redness, pain, persistent blurring
Common Problems-and How to Fix Them
No lens is perfect. Here’s what goes wrong-and how to fix it:- Foreign body sensation (45% of new wearers): Usually goes away with time. If not, your lens edge might be too thick. Ask your fitter to polish it.
- Lens fogging (25%): Caused by protein buildup. Switch to a preservative-free cleaning solution. Use enzyme tablets weekly.
- Lens decentration (15%): The lens shifts off-center. Your cornea might be too irregular. Try a larger scleral lens.
- Dry eyes (8-10%): Rigid lenses can worsen dryness. Use rewetting drops made for contact lenses. Avoid products with preservatives.
- Difficulty inserting/removing (32%): Practice with a mirror. Use a suction tool if needed. Most clinics give you a free training session.



Darren McGuff
January 8, 2026 AT 23:52As a cornea specialist for over 20 years, I’ve seen patients go from barely seeing their own hands to driving at night again-just because they found the right scleral fit. It’s not magic. It’s precision engineering meeting human resilience. The real win? Patients stop feeling like broken objects and start feeling like people again. That’s the quiet revolution happening in optometry right now.
Meghan Hammack
January 10, 2026 AT 00:43OMG I cried reading this. My sister had keratoconus and thought she’d never drive again-now she’s road-tripping across Arizona with her new sclerals. She says it’s like waking up from a dream she didn’t know she was in. Thank you for writing this.
RAJAT KD
January 11, 2026 AT 13:33Corneal cross-linking must be performed before lens fitting. Otherwise, progression continues and lenses become obsolete within months. This is non-negotiable clinical protocol.
Matthew Maxwell
January 12, 2026 AT 00:10It is deeply concerning that so many individuals are misled into believing rigid contact lenses are a cure. They are not. They are a palliative. The real issue is the medical community’s failure to prioritize early diagnosis and preventative intervention. Too many patients are being sold Band-Aids while their corneas decay.
Angela Stanton
January 13, 2026 AT 19:01Okay but let’s be real-scleral lenses are the new Tesla of eye gear. 💎✨ You’re basically putting a liquid cushion + custom optical dome on your eyeball. The Dk 200 materials? That’s like giving your cornea a five-star spa day. And the 3D scans? No more ‘try this one, nope, try this one’-it’s like Apple’s ProMotion for your eyes. 🤯
Catherine Scutt
January 13, 2026 AT 19:32I’ve worn RGP lenses for 12 years. Still hate putting them in. Still get dry eyes. But I’d rather deal with this than go blind. So yeah, it’s worth it.
Chris Kauwe
January 15, 2026 AT 17:08Let’s not romanticize this. In the West, we have access to scleral lenses and CXL. But in the Global South? A 16-year-old in rural India with keratoconus is lucky to get a pair of $5 reading glasses. This isn’t a medical breakthrough-it’s a privilege. The real failure isn’t the cornea-it’s the system that lets vision become a luxury.
Alicia Hasö
January 17, 2026 AT 05:22To anyone reading this who’s scared to try rigid lenses: You’re not weak for being nervous. You’re human. But I’ve seen too many young people give up too soon. The first week is rough. The second week is awkward. By week three? You’ll forget you’re wearing them. And then one day, you’ll look up at the stars and realize-your eyes are working again. Don’t quit before the miracle happens.
Aron Veldhuizen
January 18, 2026 AT 19:07Everyone’s acting like rigid lenses are the answer. But what about the 30% who can’t tolerate them? What about the ones who develop corneal neovascularization from poor oxygen flow? We’re ignoring the collateral damage because we want a simple solution. The truth? We’re just delaying the inevitable transplant. This isn’t progress-it’s procrastination dressed in science.
Pooja Kumari
January 19, 2026 AT 02:55I’ve been living with this for 8 years and I just want someone to understand how lonely it is. You smile when people ask if you’re okay, but inside you’re screaming because you can’t see your own child’s face clearly at bedtime. I tried every lens, every drop, every specialist. I cried in the optometrist’s chair three times before I found my sclerals. And now? I can see my daughter’s freckles. I can read her bedtime stories without squinting. I just… I just needed someone to say it’s okay to need help. Thank you for this. I’m not broken. I’m just healing.
Drew Pearlman
January 19, 2026 AT 22:55Look, I used to think I’d never see my own reflection clearly again. I was 21, working retail, and couldn’t read the price tags. I thought I’d have to quit my job, give up driving, live in blurry isolation. Then I got my first RGP lenses. It wasn’t perfect. I dropped them. I burned them with the wrong cleaner. I almost quit twice. But I kept going. Now? I’m a grad student. I read for fun. I travel. I see the aurora borealis last winter. All because I didn’t let fear win. If you’re reading this and you’re scared? Just try one more time. Your future self is already thanking you.