Breast Cancer Prevention: Practical Ways to Lower Your Risk
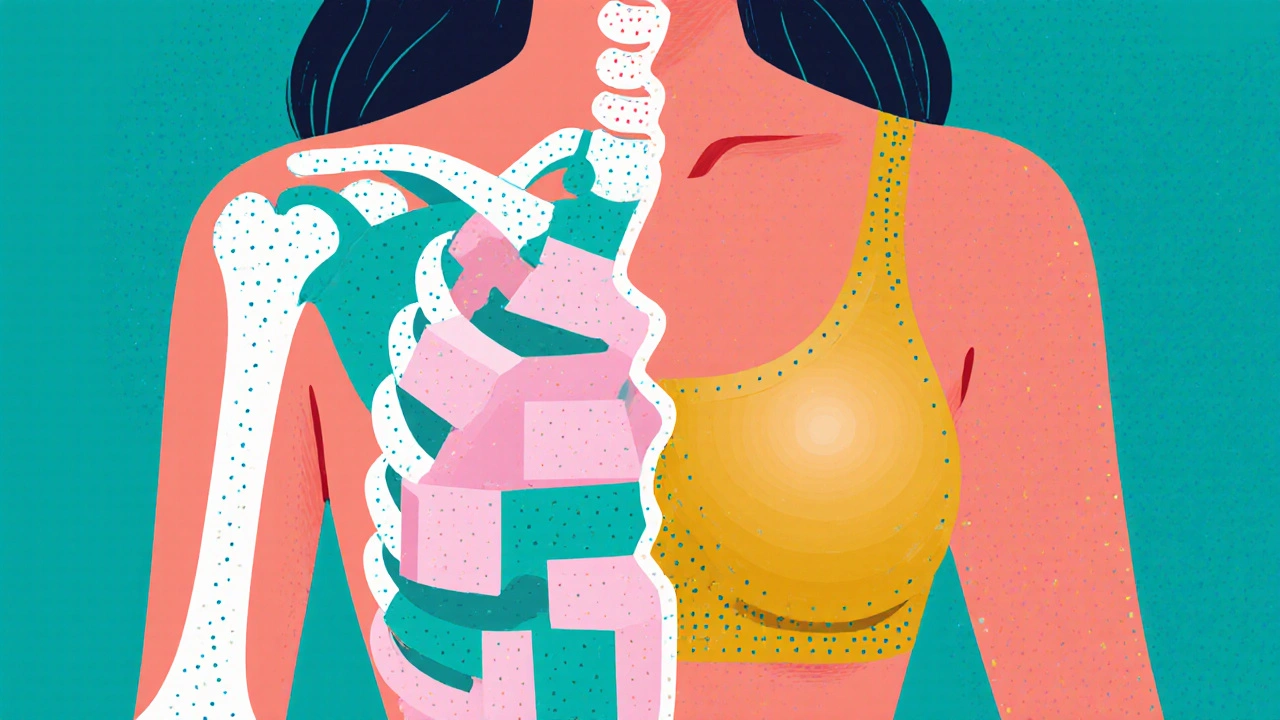
When we talk about Breast Cancer Prevention, the set of actions and habits aimed at reducing the chance of developing breast cancer. Also known as BC Prevention, it combines science, daily choices, and medical tools to keep cells healthy. Lifestyle Modification, changes in daily habits like exercise, weight control, and alcohol intake is a cornerstone, while Screening Mammography, regular imaging tests that catch early signs before symptoms appear acts as the safety net that catches what we might miss. Together they form a prevention system that reduces risk, improves early detection, and saves lives. The next sections break down how each piece fits.
Key Strategies You’ll Explore
First, breast cancer prevention thrives on lifestyle choices that influence hormone levels and inflammation. Regular aerobic exercise—aim for 150 minutes a week—lowers estrogen and insulin spikes, both linked to tumor growth. Strength training adds muscle mass, helping the body store fat more efficiently and keep body‑mass index in a healthy range. Weight control matters because excess adipose tissue produces extra estrogen, especially after menopause. Limit alcohol to no more than one drink per day; every additional drink raises risk by about 7 %. Smoking, often overlooked, damages DNA and impairs the immune system, so quitting adds another layer of protection.Dietary Choices, a diet rich in fruits, vegetables, whole grains, and healthy fats provide antioxidants and fiber that help the body detoxify potential carcinogens. Studies show that leafy greens, berries, and cruciferous vegetables like broccoli contain compounds that interrupt cancer cell signaling. Replacing red meat with fish or legumes reduces saturated fat intake, which is associated with lower inflammation. Even modest changes—adding a serving of beans or a daily smoothie—create a cumulative effect over years. These habits, when combined, create a triple‑action shield: they lower hormone exposure, cut inflammatory pathways, and boost immune surveillance.
Second, medical screening complements these habits by catching abnormal cells early. Guidelines recommend mammograms every two years for women aged 50‑74, but many experts suggest starting at 40 if you have a family history or dense breast tissue. When a mammogram finds a suspicious spot, follow‑up imaging or a biopsy can pinpoint whether it’s benign or malignant, giving doctors a head start. Genetic counseling adds another layer; if you carry BRCA1 or BRCA2 mutations, more frequent imaging or MRI may be advised. Early detection not only improves survival rates but often allows for less aggressive treatment, preserving quality of life. Finally, staying informed about new research—like the role of vitamin D, gut microbiome balance, and hormone‑blocking drugs—helps you adapt your prevention plan as science evolves. Below you’ll find a curated list of articles that dive deeper into exercise routines, nutrition tips, screening schedules, and emerging therapies, giving you actionable steps to build a personalized prevention roadmap.
Calcium Deficiency Linked to Breast Cancer Risk - Prevention Tips
Learn how calcium deficiency may raise breast cancer risk and discover diet, supplement, and lifestyle strategies to lower that risk.