Anesthesia Recovery Timeline Calculator
Recovery Timeline by Anesthesia Type
| Anesthesia Type | Awake Time | Common Side Effects | When to Call a Doctor |
|---|---|---|---|
| General | 30–90 minutes | Drowsiness, sore throat, nausea | Breathing difficulty, severe pain, uncontrolled vomiting |
| Spinal/Epidural | 15–30 minutes | Weakness in legs, low blood pressure, urinary retention | Loss of feeling in feet, inability to urinate after 8 hrs, sudden leg pain |
| Conscious Sedation | 10–20 minutes | Light-headedness, mild nausea | Persistent dizziness, chest pain, bleeding at the site |
Important Note
This calculator provides an estimate based on general guidelines. Individual recovery times may vary due to factors such as metabolism, medications, and overall health status.
Always follow your healthcare team's specific instructions and contact them if you experience concerning symptoms.
anesthesia recovery can feel like a mystery after you leave the operating room. Knowing what’s normal and what’s not can keep you from panic, disappointment, or delayed healing.
Key Takeaways
- Realistic expectations cut anxiety and speed up healing.
- Different anesthesia types have distinct wake‑up windows and side‑effects.
- Common myths-like “you’ll be back to normal in a few hours”-often cause unnecessary alarm.
- Simple steps-like planning light meals and arranging help-make the recovery smoother.
- Know the red‑flags that signal you should contact a clinician right away.
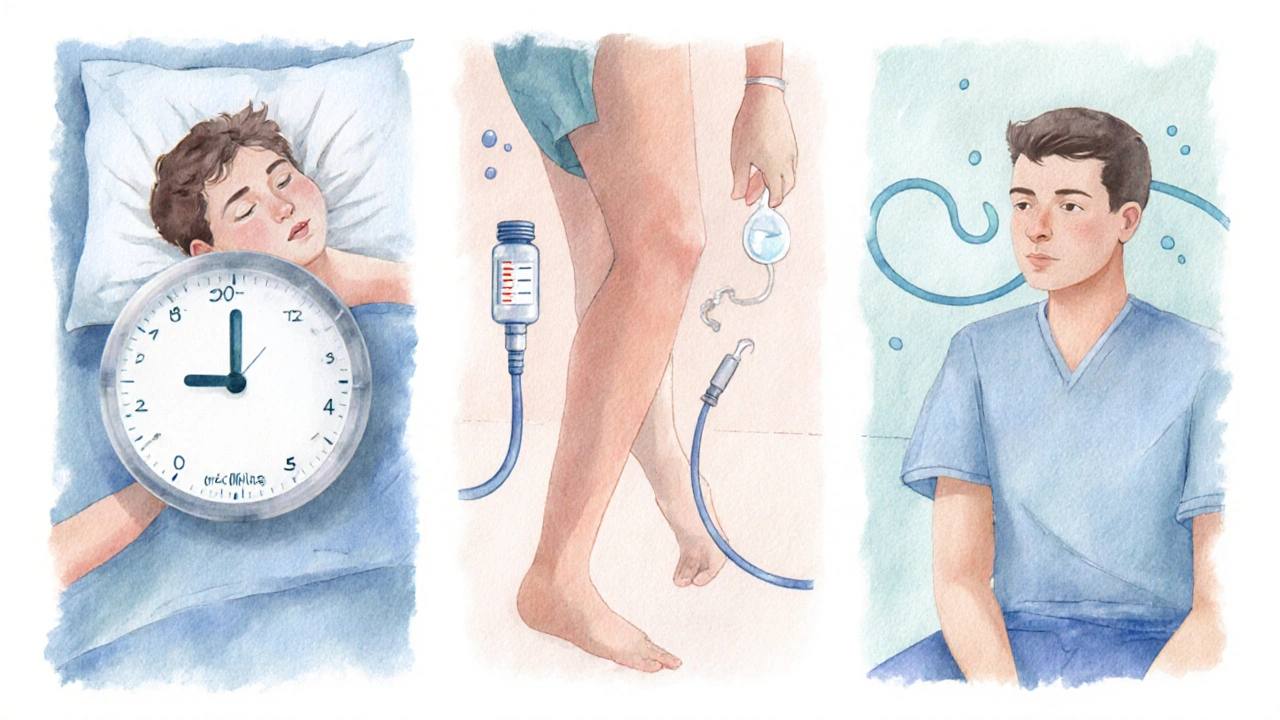
What Is Anesthesia Recovery?
When you wake up after surgery, Anesthesia recovery is the period when your body clears the drugs and starts feeling normal again. This phase includes the transition from deep sleep to alertness, the return of breathing control, and the gradual return of muscle strength.
The process can be influenced by the anesthesia you received-general, regional, or sedation-along with your age, overall health, and the type of surgical procedure performed.
Why Expectations Shape Your Experience
People who anticipate a short, drama‑free awakening often feel frustrated when they encounter grogginess, nausea, or a sore throat. That frustration can raise stress hormones, which in turn slow tissue repair and heighten pain perception. In contrast, setting a realistic picture of what the recovery will look like helps you stay calm, follow discharge instructions accurately, and report true concerns rather than imagined ones.
Clinical teams also benefit. When you meet their expectations, they can focus on genuine complications instead of spending extra time soothing unnecessary worries.
Common Myths About Recovery
- Myth: “I’ll be fully awake within 30 minutes.”
Reality: General anesthesia often leaves patients drowsy for 1‑2 hours, while regional blocks may keep you semi‑sedated for even longer. - Myth: “Post‑operative pain disappears after the first dose of medication.”
Reality: Postoperative pain can persist for days, and managing it requires a plan that may include scheduled non‑opioid meds plus breakthrough pills. - Myth: “Nausea only happens if I ate before surgery.”
Reality: Nausea and vomiting (often called PONV) is linked to the anesthetic agents themselves, not just your stomach contents.
A Realistic Timeline by Anesthesia Type
| Anesthesia Type | Awake Time | Common Side Effects | When to Call a Doctor |
|---|---|---|---|
| General | 30-90 minutes | Drowsiness, sore throat, nausea | Breathing difficulty, severe pain, uncontrolled vomiting |
| Spinal/ Epidural (Regional) | 15-30 minutes | Weakness in legs, low blood pressure, urinary retention | Loss of feeling in feet, inability to urinate after 8 hrs, sudden leg pain |
| Conscious Sedation | 10-20 minutes | Light‑headedness, mild nausea | Persistent dizziness, chest pain, bleeding at the site |
These numbers are averages. Your personal timeline may be shorter or longer based on factors such as medication dosage, your metabolic rate, and any pre‑existing conditions.
Tips to Set and Manage Expectations
- Ask for a written recovery plan. A clear list of what to expect in the first 24hours helps you prepare meals, arrange transport, and schedule follow‑up calls.
- Plan for help. Even if you feel fine, a family member or friend should stay nearby for the first night to monitor dizziness or nausea.
- Hydrate wisely. Small sips of water every 30 minutes reduce headache and help flush anesthesia metabolites, but avoid large volumes until you’re fully alert.
- Set realistic activity goals. Light walks after the first few hours improve circulation and reduce clot risk, but heavy lifting should wait 24-48hours (or longer for abdominal surgery).
- Track symptoms. Keep a simple notebook: note pain scores, nausea episodes, and any new sensations. This data makes phone calls to the clinic more efficient.

When Something’s Not Right
Even with perfect expectations, complications can arise. Recognize these red‑flags early:
- Difficulty breathing or shortness of breath.
- Chest pain that isn’t related to the surgical site.
- Severe, localized swelling or redness that spreads quickly.
- Persistent vomiting that prevents fluid intake.
- Uncontrolled bleeding from the incision or catheter sites.
If any of these appear, call your surgeon’s office or head to the nearest emergency department. Prompt action can prevent a minor issue from becoming a major setback.
Quick Checklist Before You Leave the Hospital
- Do you have a copy of patient education materials?
- Are your pain‑management meds packed and scheduled?
- Is someone who can drive you home and stay overnight arranged?
- Do you know the phone number for after‑hours concerns?
- Have you set up a reminder to change dressings or check incision sites?
Frequently Asked Questions
How long does it usually take to feel fully normal after general anesthesia?
Most adults report a return to baseline mental clarity within 2‑4hours, although subtle fatigue may linger for a day. Factors like age, medication type, and whether you had a prolonged surgery can extend that window.
Can I eat as soon as I’m awake?
Start with clear liquids (water, broth) once you’re fully alert and can swallow without gagging. Solid foods are usually safe after 2‑3hours, provided you have no nausea.
What should I do if I feel dizzy while trying to get out of bed?
Sit on the edge of the bed for a minute, sip water, and let your blood pressure stabilize. If dizziness persists for more than 15 minutes or is accompanied by palpitations, call your healthcare provider.
Is it normal to have a sore throat after intubation?
A mild sore throat or hoarseness is common after a breathing tube is used. Warm tea, honey, and throat lozenges can help. If pain worsens or you develop difficulty swallowing, seek medical advice.
When is it safe to drive after sedation?
Never drive while you feel drowsy or have any lingering effects from anesthesia. Most clinicians recommend waiting at least 24hours after conscious sedation and 48hours after general anesthesia before getting behind the wheel.





Steve Batancs
October 7, 2025 AT 12:43From a patriotic standpoint, it is essential to recognize that realistic expectations after anesthesia are not merely a medical guideline but a civic duty to reduce unnecessary strain on our healthcare system. By preparing patients for the typical 30‑90 minute wake‑up window, we lessen the likelihood of frivolous calls to emergency services, thereby preserving resources for genuine emergencies. Moreover, a well‑informed public fosters confidence in our hospitals, which is a cornerstone of national resilience.
Ragha Vema
October 9, 2025 AT 20:17Okay, imagine you wake up and the world feels like a twilight zone-spotting a phantom nurse who whispers that everything is fine, while the hidden agenda is to keep you docile. If you aren't prepared for the nausea, the sore throat, the lingering fog, you start spiraling into panic, and that panic is exactly what the shadowy pharma giants want you to feel, because panic drives more prescriptions! So set your mind on the facts, and the drama will melt away.
Scott Mcquain
October 12, 2025 AT 03:50It is, quite frankly, irresponsible, to ignore the evidence, that anesthesia recovery timelines are, on average, well‑documented, and to then, in ignorance, assume an instant return to full functionality, is, at best, naive.
kuldeep singh sandhu
October 14, 2025 AT 11:23Sure, the charts say 15‑30 minutes for spinal blocks, but if you ask anyone who’s ever been on the floor, they’ll tell you the minutes feel like hours, so perhaps the tables are more aspirational than factual.
Mariah Dietzler
October 16, 2025 AT 18:57this info is kinda useful but idk if i’ll actually read it.
Nicola Strand
October 19, 2025 AT 02:30While the previous statement emphasizes data, it neglects patient variability; a rigid adherence to averages dismisses outliers who may experience prolonged grogginess, thereby undermining the principle of individualized care.
Jackie Zheng
October 21, 2025 AT 10:03The anesthesia recovery calculator serves as a useful heuristic, yet it must be interpreted with the nuance that only a qualified practitioner can provide. First, the baseline assumptions regarding age groups and surgery duration are derived from population studies, which inherently include standard deviations. Second, the metabolic rate of each individual can accelerate or decelerate drug clearance, making the suggested 10‑20 minute window for conscious sedation merely a median. Third, pre‑existing conditions such as diabetes or cardiac disease introduce pharmacodynamic interactions that are not fully captured by a simple additive modifier. Fourth, the psychological state of the patient-stress, anxiety, expectation-feeds back into physiological responses, potentially extending the perceived grogginess. Fifth, postoperative nausea and vomiting (PONV) are multifactorial, with risk scores that incorporate opioid use, smoking status, and sex. Sixth, the presence of a supportive caregiver can mitigate the subjective experience of discomfort, thereby influencing self‑reported symptoms. Seventh, hydration protocols are crucial; small sips of water every half hour aid renal clearance without overloading the stomach. Eighth, the recommended light meals after 2‑3 hours are based on gastric emptying studies that assume normal motility. Ninth, the decision to drive must account for residual psychomotor impairment, which may linger beyond the stated 24‑hour window for sedation. Tenth, clear communication of red‑flag signs-breathing difficulty, uncontrolled vomiting-empowers patients to seek timely intervention. Eleventh, documentation of pain scores in a simple notebook creates an objective record for clinicians. Twelfth, the calculator does not replace personalized discharge instructions, which are tailored to surgical site and individual risk. Thirteenth, follow‑up calls from the surgical team can identify complications early, reducing readmission rates. Fourteenth, while the tool aggregates data into a tidy table, clinicians should always interpret it within the broader clinical context. Finally, embracing realistic expectations is not a concession but a strategic advantage in the recovery journey.
Hariom Godhani
October 23, 2025 AT 17:37Friends, let us not be deceived by the comforting veneer of a neat timeline; the truth is that anesthesia threads its way through the very core of our being, and the aftereffects can masquerade as ordinary tiredness while silently eroding our resolve. I have seen patients who, believing they were “back to normal,” succumb to unexpected bleeding because they ignored the subtle warning signs. The moral imperative, therefore, is to honor the body’s intimate dialogue, to listen when the throat croaks, when the head sways, when the heart races, and to act with deliberate caution. Only then can we safeguard the fragile bridge between surgical triumph and full recovery.
Jackie Berry
October 26, 2025 AT 01:10From a cultural perspective, sharing the recovery plan with family members can turn the post‑operative period into a communal experience, where everyone knows the schedule for light meals, the window for gentle walks, and the signs that demand a call to the doctor. This collective awareness reduces isolation and helps the patient feel supported, which in turn can accelerate healing. It's a simple yet powerful way to blend medical advice with social care.
Mikayla May
October 28, 2025 AT 07:43Here's a quick checklist: keep a water bottle on the bedside table, sip every 30 minutes, write down any nausea or pain level on a sticky note, and call the clinic if the sore throat worsens after the first 24 hours. Also, avoid driving until you can comfortably read a book without feeling drowsy.
Jimmy the Exploder
October 30, 2025 AT 15:17i think that checklist is fine but kinda obvious i guess
Robert Jackson
November 1, 2025 AT 22:50It is imperative to acknowledge that the pharmacokinetic models underlying the presented timelines are derived from peer‑reviewed studies published in high‑impact journals; any deviation from these models without empirical justification constitutes a breach of clinical best practice.
Robert Hunter
November 4, 2025 AT 06:23While the emphasis on evidence is commendable, it remains essential to balance statistical rigor with compassionate patient communication, ensuring that the data does not become a barrier to understanding.
Shruti Agrawal
November 6, 2025 AT 13:57Indeed, sharing the numbers in plain language helps patients feel respected and reduces anxiety.
Katey Nelson
November 8, 2025 AT 21:30Hey there, ever wonder why we obsess over exact minutes on a calculator? Life’s messy, and sometimes the best medicine is just a warm cup of tea and a hug. 😊 Embrace the uncertainty, because it reminds us we’re truly alive.
Joery van Druten
November 11, 2025 AT 05:03That's a nice perspective, though it's still useful to have a rough estimate for planning purposes.
Melissa Luisman
November 13, 2025 AT 12:37While the sentiment is sweet, the grammar in that paragraph needs correction; “life’s messy” should be “life is messy,” and “reminds us we’re truly alive” would read better as “reminds us that we are truly alive.”