Most people think of painkillers like ibuprofen or acetaminophen as harmless, everyday fixes. You’ve got a headache? Pop two. Back pain flaring up? Take one before bed. But what if those pills, taken over years, are quietly damaging your kidneys? This isn’t speculation-it’s analgesic nephropathy, a preventable form of chronic kidney disease caused by long-term use of common pain medications.
What Exactly Is Analgesic Nephropathy?
Analgesic nephropathy isn’t a sudden injury. It’s a slow, silent erosion of kidney tissue from taking too many painkillers over time. The damage builds up quietly, often without symptoms until the kidneys are already failing. The main culprits are NSAIDs-like ibuprofen, naproxen, and aspirin-and acetaminophen, especially when used daily for years.
Back in the 1970s and 80s, this condition was more common because many over-the-counter pain relievers contained phenacetin, a now-banned ingredient linked to severe kidney damage. Today, phenacetin is gone, but the problem hasn’t disappeared. Instead, people are now getting kidney damage from the same habits-just with different drugs.
The kidneys work hard to filter blood and regulate fluid balance. NSAIDs block enzymes that help keep blood flowing to the kidneys. When you take them daily, that blood flow drops by 25-40%. Over time, this starves kidney tissue of oxygen, leading to cell death, scarring, and loss of function. Acetaminophen, while less harmful to the kidneys than NSAIDs, still contributes when taken in large doses over years-especially above 3,000 mg daily.
Who’s at Risk?
This isn’t just about people who take 10 pills a day. It’s about consistent, long-term use. People most at risk:
- Women over 30, especially those managing chronic headaches, menstrual pain, or arthritis
- People over 45
- Those with existing high blood pressure, diabetes, or early kidney disease
- Anyone taking combination pain relievers (like Excedrin, which has aspirin, acetaminophen, and caffeine)
Studies show that people who take six or more pain pills a day for three or more years have a dramatically higher risk. And here’s the kicker: combination products with caffeine or codeine are 3.7 times more likely to cause kidney damage than single-ingredient pills.
Women make up 72% of diagnosed cases. Why? Many are self-managing chronic pain-migraines, back pain, fibromyalgia-without realizing the long-term cost. A Reddit user from 2023 shared: "I took 8-10 Excedrin Migraine tablets daily for seven years before my GFR dropped to 45. My nephrologist said I was lucky it wasn’t worse."
How Do You Know If It’s Happening to You?
Here’s the scary part: you probably won’t feel anything until it’s advanced. Early stages show no symptoms. That’s why routine blood tests are critical.
Doctors look for:
- Elevated serum creatinine (a waste product that builds up when kidneys slow down)
- Low estimated glomerular filtration rate (eGFR) below 60
- Non-nephrotic proteinuria (small amounts of protein in urine)
- Bland urinary sediment (no red blood cells or casts, which rules out other kidney diseases)
Advanced cases show high blood pressure, anemia, and swelling in the legs. Late-stage signs include flank pain, blood in urine, or even passing pieces of dead kidney tissue (papillae) that can block the urinary tract.
Noncontrast CT scans can spot calcified renal papillae-signs of advanced damage-with 87% sensitivity. But by the time those appear, the damage is already severe.

How Common Is This?
In Australia during the peak of phenacetin use, analgesic nephropathy caused up to 10% of all end-stage kidney disease cases. Today, that number has dropped-but the problem is still growing under the radar.
In the U.S., it’s responsible for 2-3% of all chronic kidney disease cases, or about 15,000-20,000 new cases every year. That’s not a small number. And it’s preventable.
What’s worse? A 2022 Cedars-Sinai survey found that 62% of patients didn’t believe over-the-counter painkillers could hurt their kidneys. That myth is costing people their kidney function.
NSAIDs vs. Acetaminophen: Which Is Safer?
People often assume acetaminophen (Tylenol) is the "safe" choice for kidneys. It’s better than NSAIDs-but not risk-free.
A 2020 study in Kidney International Reports found that taking more than 4,000 mg of acetaminophen daily for five years increased chronic kidney disease risk by 68% compared to non-users. That’s not a typo. That’s one pill every four hours, every day, for five years.
NSAIDs are worse. They reduce kidney blood flow directly. Even at normal doses, they can trigger acute kidney injury in vulnerable people. Chronic use leads to irreversible scarring.
Here’s the reality: neither is truly safe for daily, long-term use. The difference is one is more dangerous than the other.
What Can You Use Instead?
Stopping NSAIDs and acetaminophen cold turkey can leave people in pain. But there are better options.
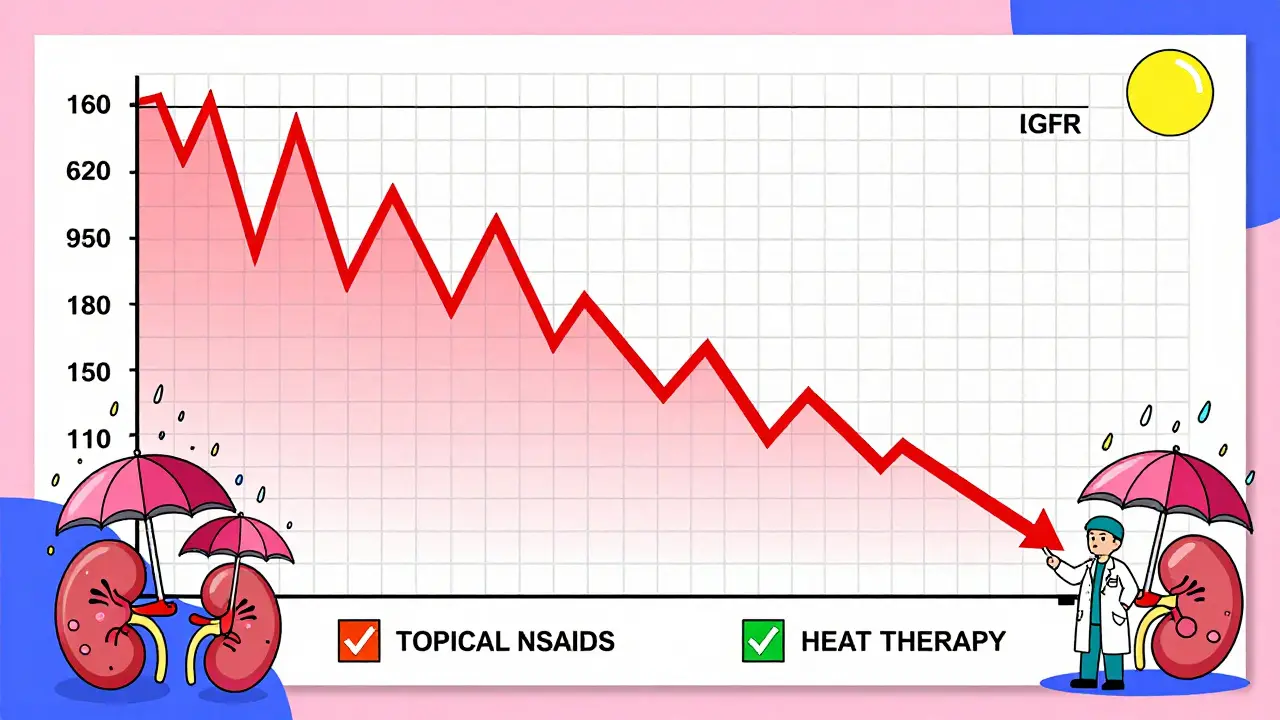
1. Topical NSAIDs
Instead of swallowing pills, try gels or patches. A 2021 trial in Arthritis & Rheumatology showed topical diclofenac provided the same pain relief as oral NSAIDs for osteoarthritis-but with no drop in kidney function. That’s because less than 10% of the drug enters your bloodstream.
2. Heat Therapy
Heat wraps like ThermaCare have FDA clearance for pain relief without drugs. Studies show they reduce osteoarthritis pain by 40-60%. They’re safe for kidneys, easy to use, and work well for back, neck, and joint pain.
3. Physical Therapy and Movement
The American College of Rheumatology recommends trying physical therapy, stretching, or low-impact exercise for 4-6 weeks before turning to any painkiller. For many, this alone reduces pain enough to avoid pills entirely.
4. Cognitive Behavioral Therapy (CBT)
Chronic pain isn’t just physical-it’s neurological. CBT helps retrain how your brain processes pain signals. Studies show it reduces pain intensity by 30-50% in people with migraines, fibromyalgia, and chronic back pain.
5. Prescription Alternatives
For migraine sufferers, CGRP inhibitors (like Aimovig or Emgality) are now available. They’re expensive-around $650 a month-but they don’t touch your kidneys at all. For arthritis, duloxetine (Cymbalta) is sometimes used off-label and has no renal risk.
What Should You Do Now?
Here’s your action plan:
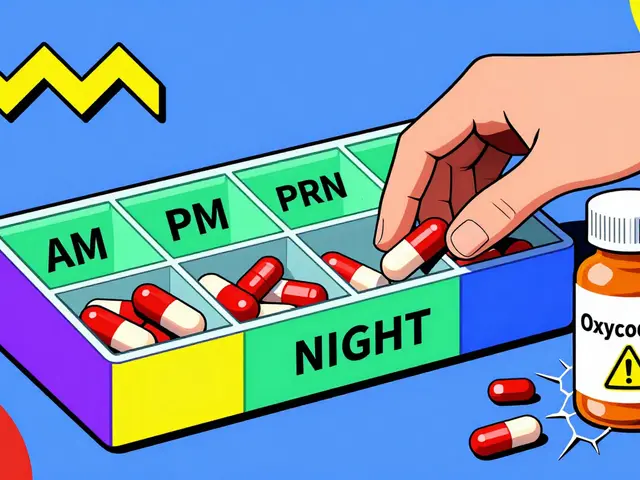
- Count your pills. How many NSAIDs or acetaminophen do you take per week? If it’s more than three days, you’re in the risk zone.
- Stop combination products. Ditch Excedrin, Midol, and similar mixtures. They’re more dangerous than single-ingredient pills.
- Set hard limits. Never exceed 3,000 mg of acetaminophen daily. Never take NSAIDs daily for more than 10 days without talking to your doctor.
- Ask for a blood test. Request a serum creatinine and eGFR check at your next visit-even if you feel fine.
- Try non-drug options. Start with heat, movement, or stretching. If pain persists, ask about topical NSAIDs or CBT.
One 2022 study followed 142 people who stopped analgesics after early diagnosis. Seventy-three percent stabilized their kidney function and never declined further. That’s not a miracle-it’s prevention.
Why This Matters More Than You Think
Kidney disease doesn’t just mean dialysis. It means fatigue, high blood pressure, bone problems, heart disease, and a lifetime of restrictions. The cost? Up to $90,000 per year for dialysis. For early-stage management? Still $18,500 a year.
And yet, the FDA mandated stronger warning labels on NSAID packaging in 2020. Major manufacturers like Bayer and Johnson & Johnson have reduced acetaminophen and caffeine in their combo products. But awareness hasn’t caught up.
Most people still don’t know that their daily painkiller habit could be slowly killing their kidneys. This isn’t about fear-it’s about awareness. You don’t need to suffer in pain. You just need better tools.
Can you reverse analgesic nephropathy?
If caught early-before major scarring occurs-stopping the painkillers can stop further damage. In 73% of cases studied, kidney function stabilized after discontinuing NSAIDs and acetaminophen. But once the tissue is scarred, it doesn’t heal. Prevention is the only cure.
Is Tylenol safe for kidneys?
Acetaminophen (Tylenol) is less harmful to kidneys than NSAIDs, but it’s not safe with long-term daily use. Taking more than 3,000 mg per day for five years increases chronic kidney disease risk by 68%. Stick to the lowest dose needed for the shortest time.
What’s the safest painkiller for someone with kidney disease?
There’s no perfect oral painkiller for people with existing kidney disease. Topical NSAIDs are the safest option for localized pain. For widespread pain, non-drug methods like heat, physical therapy, or CBT are preferred. Always consult a nephrologist before taking any new medication.
How long does it take for NSAIDs to damage kidneys?
Damage can start within months of daily use, but it usually takes years to become noticeable. The risk increases sharply after three years of taking six or more pills per day. That’s why early detection through blood tests is critical.
Should I stop taking ibuprofen if I have high blood pressure?
Yes. NSAIDs like ibuprofen raise blood pressure and reduce kidney blood flow-two things that worsen kidney damage in people with hypertension. Use acetaminophen sparingly, or better yet, try topical NSAIDs, heat therapy, or physical therapy instead.



Sally Dalton
January 26, 2026 AT 08:36I had no idea my daily Excedrin habit was slowly killing my kidneys... I took 8-10 a day for years because my migraines were unbearable. My doctor just told me last month my eGFR is 52. I'm terrified but also so relieved I found this post. Time to ditch the pills and try heat wraps and PT. Thanks for the wake-up call.
Betty Bomber
January 27, 2026 AT 21:04Wow. Just... wow. I've been taking ibuprofen every night for back pain since college. 15 years. I'm 41 now. I'm gonna get my bloodwork done next week. No more excuses.
Mohammed Rizvi
January 28, 2026 AT 22:10So let me get this straight - we’ve got a silent killer hiding in plain sight in every pharmacy aisle, and the FDA’s idea of a warning is a tiny footnote no one reads? And people still think Tylenol is ‘safe’? The real tragedy isn’t the kidney damage - it’s that we’ve normalized self-medication like it’s yoga.
Nicholas Miter
January 29, 2026 AT 08:28My grandma took 4 Tylenol a day for 20 years for her arthritis. She never had kidney issues - but she also never had high blood pressure or diabetes. Context matters. Not everyone’s at risk. But yeah, if you’re taking painkillers daily, you’re playing Russian roulette with your nephrons.
Topical diclofenac changed my life. No stomach upset, no kidney stress. Just slap it on and move on.
Rakesh Kakkad
January 30, 2026 AT 08:10Respected sir/madam, I am from India and I must say that this article is extremely informative and scientifically accurate. In our country, people consume NSAIDs like candy, especially during fever and headache. We must educate the masses through community health workers and local pharmacies. I have already shared this article with my neighborhood clinic. Thank you for your noble work.
Ryan W
February 1, 2026 AT 06:03Let’s be real - this is just another fearmongering piece dressed up as medical advice. The data is cherry-picked. People who take 10 pills a day for 7 years are outliers. Most people take 1-2 occasionally. The real threat is misinformation, not ibuprofen. Also, CBT? For pain? Next you’ll say meditation cures cancer.
George Rahn
February 3, 2026 AT 03:28Every time I see one of these articles, I think: America’s problem isn’t painkillers - it’s the refusal to tolerate discomfort. We’ve turned into a nation of fragile, over-medicated zombies who can’t sit with a headache. You want relief? Move. Breathe. Endure. Your body isn’t a vending machine.
Napoleon Huere
February 4, 2026 AT 13:56Think about it - we’re told to drink 8 glasses of water a day to stay healthy, but no one tells us that popping a pill every day is like pouring acid into your organs. We treat our bodies like disposable devices. But kidneys? They don’t come with a warranty. Once they’re gone, you’re just waiting for the battery to die.
Geoff Miskinis
February 5, 2026 AT 15:45As a nephrologist, I can confirm this is accurate. But I’m also tired of patients blaming the medication. The real issue is the lack of primary care access. If people had access to physical therapists, pain specialists, and mental health resources, they wouldn’t be self-medicating with OTC pills in the first place. This isn’t about education - it’s about systemic failure.
SWAPNIL SIDAM
February 5, 2026 AT 21:53I am from India and I take only paracetamol when I have headache. I never take ibuprofen. I am happy to know that I am doing right. Thank you for sharing this.
Shawn Raja
February 7, 2026 AT 05:29So you’re telling me the same pills I’ve been using since high school to get through finals, work shifts, and my mom’s funeral are slowly turning my kidneys into gravel? And the FDA’s solution is a tiny label? I’m not mad - I’m just disappointed. We’ve been sold a lie wrapped in a plastic bottle labeled ‘safe for daily use.’ The real painkiller isn’t the pill - it’s the courage to stop and ask: ‘Why am I in so much pain?’