Imagine feeling a burning sensation after every meal, and then learning that the same irritation could turn the lining of your food pipe into a pre‑cancerous state. That’s the reality for many people living with chronic acid reflux. Below we break down what GERD is, how it can lead to Barrett’s Esophagus, and what you can do to keep the progression in check.
What Exactly Is GERD?
When the stomach’s acid continuously flows back into the esophagus, GERD is a chronic condition that causes heartburn, regurgitation, and sometimes chest pain. The lower esophageal sphincter (LES) normally acts like a one‑way valve, but in GERD it either relaxes too often or weakens, allowing gastric contents to splash upward.
- Common triggers: fatty meals, caffeine, alcohol, smoking, and tight clothing.
- Typical symptoms: burning behind the breastbone, sour taste, chronic cough, hoarseness.
- Long‑term risks: esophagitis, strictures, and Barrett’s Esophagus.
Studies from Australian gastroenterology centres show that roughly 15% of adults report weekly heartburn, and about a third of those meet the diagnostic criteria for GERD.
Barrett’s Esophagus: When the Esophagus Starts to Change
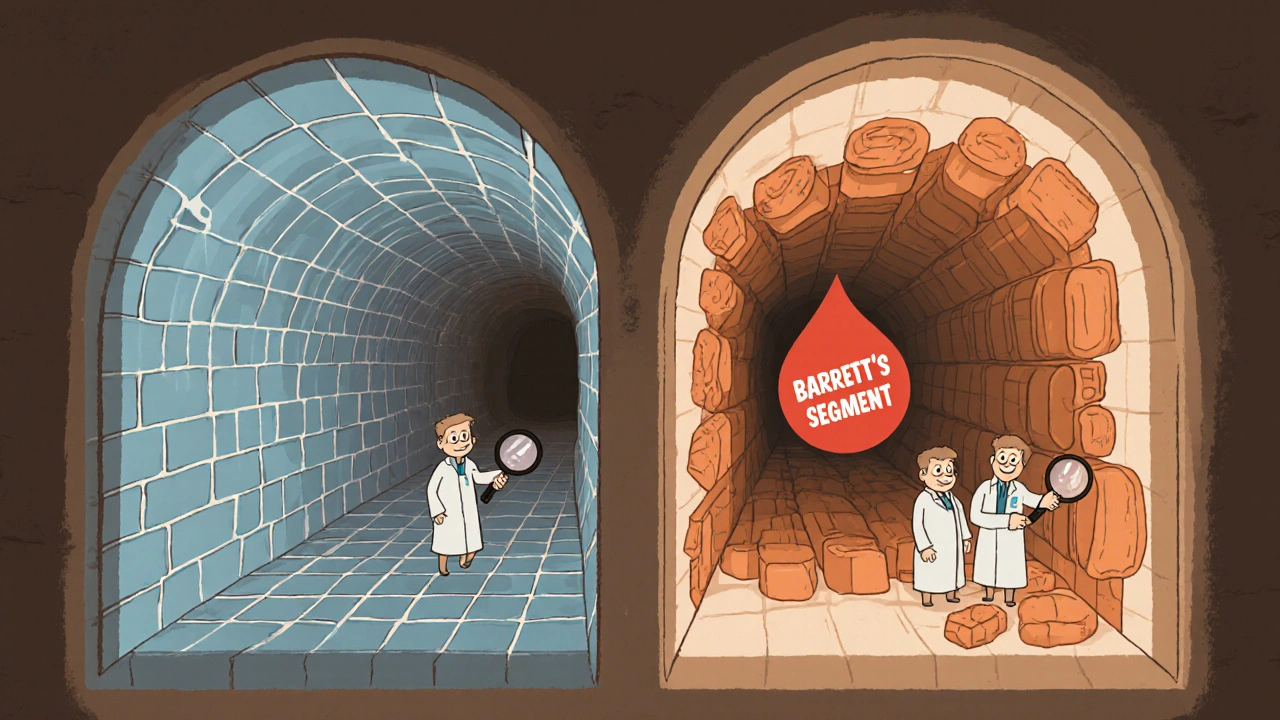
Barrett’s Esophagus is a condition where the normal squamous cells lining the esophagus are replaced by columnar cells, similar to those in the stomach or intestine. This process, called intestinal metaplasia, occurs as a protective response to chronic acid exposure.
Barrett's Esophagus is considered a pre‑cancerous stage because the altered cells have a higher chance of turning into esophageal adenocarcinoma.- Incidence: about 5‑10% of people with longstanding GERD develop Barrett’s.
- Risk factors: male gender, age over 50, obesity, smoking, and a family history of esophageal cancer.
- Symptoms are often silent; many discover it during an endoscopy for unrelated reasons.
How GERD Leads to Barrett’s - The Pathophysiology
Repeated acid attacks damage the esophageal lining, prompting inflammation (esophagitis). The body attempts to shield itself by replacing the delicate squamous cells with tougher columnar cells. Over years, this adaptation becomes permanent, creating the characteristic “Barrett’s segment.”
Data from a 2023 longitudinal cohort in Sydney showed that patients with daily heartburn for more than 5years had a 12‑fold increased odds of developing Barrett’s compared with those whose symptoms were well‑controlled.
Diagnosing the Complication - What Tests Are Used?
Because Barrett’s often hides behind silent symptoms, physicians rely on screening tools, especially for high‑risk individuals.
| Tool | What It Detects | Invasiveness | Typical Use |
|---|---|---|---|
| Upper Endoscopy (EGD) | Barrett’s segment, esophagitis, early cancer | Invasive (sedation required) | Screening for high‑risk GERD patients |
| Bravo™ pH Monitoring | Acid exposure time over 24h | Minimally invasive (capsule) | Confirming uncontrolled reflux |
| Manometry | LES pressure and motility | Minimally invasive (catheter) | Pre‑surgical evaluation |
| Barium Swallow | Structural abnormalities, strictures | Non‑invasive (X‑ray) | Initial assessment when endoscopy not available |
The gold‑standard remains the esophagogastroduodenoscopy (EGD). Esophagogastroduodenoscopy allows direct visualization and biopsy of suspicious tissue, confirming the presence of intestinal metaplasia.
Managing GERD to Prevent Barrett’s Progression
Addressing reflux early can halt or even reverse the metaplastic changes in some patients.
- Lifestyle tweaks
- Lose 5‑10% of body weight if BMI>30.
- Avoid meals within 2‑3hours of bedtime.
- Elevate the head of the bed 10‑15cm.
- Medication options
- Proton pump inhibitors (PPIs) suppress acid production and heal erosive esophagitis; they are first‑line for chronic GERD.
- H2‑blockers (e.g., ranitidine alternatives) work slower but are useful for intermittent symptoms.
- Alginate formulations form a foamy barrier that can reduce breakthrough reflux.
- Surgical considerations
- Laparoscopic fundoplication restores LES tone for patients who fail medical therapy.
- Magnetic sphincter augmentation (LINX) offers a reversible, less‑invasive alternative.
When Barrett’s is already present, regular surveillance endoscopy is recommended to catch dysplasia early.
Surveillance endoscopy is usually performed every 3‑5years for non‑dysplastic Barrett’s, shortening to 6‑12months if low‑grade dysplasia appears.
From Barrett’s to Esophageal Cancer - Reducing the Risk
While the absolute risk of progressing from Barrett’s to adenocarcinoma is low (about 0.5% per year), it’s still the most concerning complication.
- Control reflux aggressively; PPIs have been shown to reduce progression rates by up to 50% in some cohorts.
- Endoscopic therapies such as radiofrequency ablation (RFA) can eradicate dysplastic tissue, resetting the lining to normal squamous cells.
- Maintain a diet rich in fruits, vegetables, and soluble fiber; studies link these foods to lower esophageal cancer incidence.
Patients diagnosed with high‑grade dysplasia often undergo endoscopic mucosal resection followed by RFA, achieving 90% remission rates.
Key Takeaways
- GERD is the leading driver of Barrett’s Esophagus; long‑standing, uncontrolled reflux raises the odds dramatically.
- Barrett’s often shows no symptoms; screening endoscopy is the only reliable way to detect it early.
- Lifestyle changes, weight loss, and proper medication can halt the metaplastic process.
- Regular surveillance and, when needed, endoscopic ablation keep the cancer risk low.
- Talk to a gastroenterologist if you have daily heartburn for more than six months, especially if you’re over 50 or carry other risk factors.
Frequently Asked Questions
Can Barrett’s Esophagus be reversed?
Yes, in many cases. Aggressive acid control with PPIs and endoscopic therapies such as radiofrequency ablation can convert columnar tissue back to normal squamous cells, especially when dysplasia is absent or low‑grade.
How often should someone with Barrett’s get an endoscopy?
For non‑dysplastic Barrett’s, guidelines recommend an endoscopy every 3‑5years. If low‑grade dysplasia is found, the interval shortens to 6‑12months, and high‑grade dysplasia may require treatment within 3months.
Are there natural remedies that help GERD?
Lifestyle measures-weight loss, avoiding trigger foods, elevating the head of the bed-are the most effective “natural” steps. Some people find relief with aloe vera juice or deglycyrrhizinated licorice, but these should complement, not replace, medical therapy.
What’s the difference between GERD and occasional heartburn?
Occasional heartburn is a transient symptom that resolves on its own. GERD is a chronic condition where reflux occurs at least twice a week, causing persistent discomfort and potential esophageal injury.
Is surgery a cure for GERD?
Surgery, such as laparoscopic fundoplication, can restore LES function and eliminate dependence on medication for many patients. However, success rates vary, and some individuals may still need acid‑suppressing drugs afterward.





Johnny X-Ray
October 15, 2025 AT 13:14Wow, reading about GERD and Barrett’s feels like stepping into a drama where the hero fights fire with fire! :) Your breakdown makes the scary stuff feel doable, and I’m feeling hopeful that a few lifestyle tweaks can keep that acid monster at bay. The way you highlighted weight loss and bedtime elevation is pure gold – those are the plot twists we need. Keep the optimism coming, because every small victory against heartburn is a win for the whole cast! 🌟
tabatha rohn
October 16, 2025 AT 17:01Honestly, the article glosses over how disastrous uncontrolled reflux can become – it’s not just a mild inconvenience, it’s a ticking time bomb. The stats about a 12‑fold increase should have been shouted louder, not tucked into a paragraph. You need to hammer the point home that ignoring daily heartburn is pure negligence. 😤
Sangeeta Birdi
October 17, 2025 AT 20:48I totally get how overwhelming this can feel, especially when the symptoms are silent. 💙 It’s reassuring to know that regular endoscopies can catch changes early, and that there are real options like RFA to turn back the clock. Keep the supportive tone – it helps those of us navigating this maze feel less alone. 🙏
Chelsea Caterer
October 19, 2025 AT 00:34Weight loss matters, but dont forget to watch the coffee and tight belts. It’s a simple change that can shift the whole reflux story.
Lauren Carlton
October 20, 2025 AT 04:21The article incorrectly uses “The gold‑standard remains the esophagogastroduodenoscopy (EGD).” – it should be “remains the gold standard” without the hyphen. Also, “a 0.5% per year” would be clearer as “0.5 % per year”. Precision matters when discussing medical facts.
Katelyn Johnson
October 21, 2025 AT 08:08Great info everyone lets keep sharing tips like eating smaller meals and raising the head of the bed together we can all beat GERD
Laneeka Mcrae
October 22, 2025 AT 11:54Look, the science is clear: chronic acid exposure changes the cell lineage, and once Barrett’s sets in, surveillance becomes non‑negotiable. If you’re over 50 with obesity, you’re basically in the high‑risk bucket – no excuses. PPIs aren’t just for comfort; they actually reduce progression risk by up to half in studies.
Kendra Barnett
October 23, 2025 AT 15:41Remember, you don’t have to tackle this alone. Talk to a gastroenterologist, get a clear plan, and stick to the lifestyle tweaks. Small steps add up, and soon you’ll notice the burn fading.
Warren Nelson
October 24, 2025 AT 19:28I’ve been dealing with occasional heartburn for years, and the biggest game‑changer for me was moving dinner to earlier in the evening. Coupled with a modest weight loss and a few minutes of bedtime elevation, the night‑time reflux practically vanished. It’s wild how such simple shifts can silence the relentless burn.
Jennifer Romand
October 25, 2025 AT 23:14Ah, the elegant tapestry of gastro‑intestinal pathology unfurls before our very eyes, each acid droplet a brushstroke upon the canvas of the esophagus. One cannot help but marvel at the symphonic interplay between sphincteric incompetence and cellular metamorphosis.
Kelly kordeiro
October 27, 2025 AT 02:01In the realm of gastroenterology, the progression from gastro‑oesophageal reflux disease to Barrett’s esophagus represents a paradigm of maladaptive physiological response. Chronic exposure of the esophageal mucosa to gastric acid precipitates an inflammatory cascade, wherein cytokines such as interleukin‑8 and tumor necrosis factor‑α orchestrate epithelial injury. The ensuing reparative mechanisms invoke a phenotypic shift from stratified squamous epithelium to columnar metaplasia, a process termed intestinal metaplasia, which ostensibly confers resistance to acid injury. Nonetheless, this adaptive advantage is double‑edged, for the columnar phenotype harbours a predisposition toward dysplastic transformation. Epidemiological studies consistently demonstrate that approximately 5 to 10 % of patients with long‑standing GERD will develop Barrett’s esophagus, underscoring the clinical significance of vigilant surveillance. Endoscopic examination, complemented by targeted biopsies, remains the gold standard for definitive diagnosis, enabling histopathological confirmation of goblet cell presence. Moreover, the advent of advanced imaging modalities, such as narrow‑band imaging and confocal laser endomicroscopy, has refined the detection of subtle dysplastic lesions. Therapeutic interventions, ranging from high‑dose proton pump inhibitors to endoscopic ablative techniques, have been shown to mitigate the risk of neoplastic progression. Notably, radiofrequency ablation achieves remission rates exceeding 90 % in patients with low‑grade dysplasia, thereby restoring a semblance of normalcy to the esophageal lining. Surgical options, including laparoscopic fundoplication and magnetic sphincter augmentation, provide durable reflux control for refractory cases, albeit with variable long‑term outcomes. Lifestyle modifications, encompassing weight reduction, dietary adjustments, and nocturnal head‑of‑bed elevation, constitute the cornerstone of a comprehensive management strategy. Patient education remains paramount, for informed individuals are more likely to adhere to surveillance protocols and therapeutic regimens. In sum, the convergence of meticulous endoscopic surveillance, tailored pharmacologic therapy, and judicious surgical consideration constitutes a multifaceted approach to curbing the malignant potential inherent in Barrett’s esophagus. It is incumbent upon clinicians to remain abreast of evolving guidelines, thereby ensuring optimal patient outcomes. Future research into molecular biomarkers promises to further personalize surveillance intervals.
Chris Fulmer
October 28, 2025 AT 05:48It’s fascinating how a balanced diet rich in fiber and antioxidants can subtly diminish reflux severity, while also supporting overall gut health. I love that the piece highlights both medical and lifestyle avenues, creating a comprehensive roadmap.
William Pitt
October 29, 2025 AT 09:34Take action early and you’ll thank yourself later.