Asthma Exercise Capacity Estimator
Your Current Health Status
How This Works
Based on clinical studies (2020-2024), pulmonary rehabilitation shows significant improvements for asthma patients. Our calculator uses average results from real-world programs to estimate your potential gains.
Key Benefits:
- 14% average increase in FEV1 (vs. 3% with standard care)
- 110m average improvement in 6-minute walk distance (vs. 30m with standard care)
- 27% reduction in hospital admissions
Your Estimated Improvement
Imagine being able to climb a flight of stairs without that familiar tight‑chest panic. For many people with asthma, that feeling seems out of reach, but a structured pulmonary rehabilitation program can turn it into reality.
What is Pulmonary Rehabilitation?
When we talk about Pulmonary Rehabilitation is a multidisciplinary program that blends exercise training, education, and behavior‑change techniques to improve the physical and emotional condition of individuals with chronic respiratory diseases. The approach was first built for chronic obstructive pulmonary disease (COPD) patients, but clinicians quickly realized its value for asthma, especially when symptoms persist despite optimal medication.
Why Asthma Patients Need It
Asthma is a chronic inflammatory disease of the airways that triggers recurring episodes of wheeze, breathlessness, chest tightness, and coughing. While inhalers control inflammation, they don’t address the de‑conditioning that builds up when people avoid activity out of fear. Over time, reduced stamina and weakened respiratory muscles make everyday tasks feel harder, creating a vicious cycle of inactivity and worsening symptoms.
Pulmonary rehabilitation breaks that cycle by:
- Improving lung function through targeted breathing exercises.
- Boosting quality of life scores as patients regain confidence in their bodies.
- Teaching proper inhaler technique so medication reaches the airways more efficiently.
- Providing a supportive healthcare team environment where physiotherapists, respiratory nurses, and educators collaborate.
Core Components of an Asthma‑Focused Rehab Program
Each program is customized, but most share five pillars:
- Exercise Training: Aerobic workouts (walking, cycling, swimming) combined with resistance work to strengthen the diaphragm and intercostal muscles.
- Breathing Exercises: Techniques like diaphragmatic breathing, pursed‑lip breathing, and the Buteyko method reduce hyperventilation and improve carbon‑dioxide tolerance.
- Patient Education: Sessions cover asthma triggers, medication adherence, and self‑monitoring tools such as peak flow meters.
- Psychosocial Support: Group discussions address anxiety, depression, and the fear of exercise that often accompany chronic asthma.
- Outcome Monitoring: Regular spirometry tests and questionnaire scores track progress.
Step‑by‑Step: What to Expect in Your First 12 Weeks
Week 1-2: Assessment & Goal Setting
- Baseline spirometry, 6‑minute walk test, and symptom diary.
- Individual goal setting (e.g., “walk 2 km without wheeze”).
Week 3-6: Building Foundations
- Two supervised exercise sessions per week, focusing on low‑intensity aerobic activity.
- Daily home practice of diaphragmatic breathing for 5‑10 minutes.
- First education workshop on trigger identification.
Week 7-9: Intensifying Effort
- Introduce interval training (short bursts of higher intensity).
- Resistance training targeting core and upper‑body muscles.
- Second workshop on inhaler technique and spacer use.
Week 10-12: Consolidation & Transition
- Self‑management plan finalization.
- Repeat outcome measures to compare against baseline.
- Discussion on maintaining gains after the program ends.
Evidence: Real‑World Outcomes for Asthma Patients
Several studies published between 2020 and 2024 provide solid numbers:
- A 2022 randomized trial of 150 asthma patients showed a 14 % increase in forced expiratory volume in 1 second (FEV1) after 8 weeks of rehab, compared with a 3 % change in the control group.
- Quality‑of‑life scores (Asthma Quality of Life Questionnaire) improved by an average of 1.2 points on a 7‑point scale, surpassing the minimal clinically important difference of 0.5.
- Hospital admissions for severe asthma attacks dropped by 27 % in the year following completion of a rehab program.
Beyond numbers, patients report feeling “less scared of exercise” and notice that daily chores-like gardening or climbing stairs-no longer trigger panic.
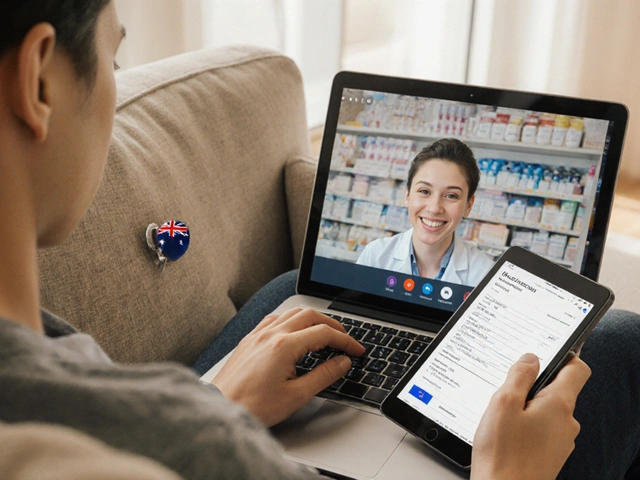
How to Find a Pulmonary Rehabilitation Program Near You
In Australia, most major hospitals and some community health centers run accredited programs. Here’s a quick checklist to verify credibility:
- Program is staffed by a certified respiratory physiotherapist.
- It includes at least three of the five core components listed above.
- Outcome monitoring uses standardized tools (spirometry, 6‑minute walk test, validated questionnaires).
- Insurance or Medicare coverage is confirmed before enrollment.
Ask your asthma specialist for a referral; they can often arrange a fast‑track entry if your symptoms are uncontrolled.

Tips to Maximize Your Rehab Benefits
- Be consistent: Missing more than two sessions a week reduces the training effect.
- Log symptoms: Tracking wheeze episodes helps the team adjust your plan.
- Practice breathing daily: Even on rest days, 5‑minute sessions reinforce muscle memory.
- Stay hydrated: Proper hydration aids mucociliary clearance and lung elasticity.
- Engage with peers: Sharing experiences reduces anxiety and builds motivation.
Comparison of Standard Asthma Care vs. Pulmonary Rehabilitation
| Outcome | Standard Care | Pulmonary Rehabilitation |
|---|---|---|
| FEV1 change | +3 % | +14 % |
| 6‑minute walk distance | +30 m | +110 m |
| Hospital admission rate (per 100 pts) | 12 | 8 |
| Asthma QoL score improvement | +0.4 | +1.2 |
| Patient‑reported confidence in exercise | Low | High |
Frequently Asked Questions
Is pulmonary rehabilitation safe for people with moderate asthma?
Yes. Programs are supervised by respiratory physiotherapists who adjust intensity based on each participant’s symptoms and spirometry results. Most people complete the program without worsening attacks.
Do I need a physician’s referral?
In Australia, Medicare usually requires a referral from a GP or asthma specialist. The referral also helps the rehab team understand your medication regimen.
How long does a typical program last?
Most programs run 8‑12 weeks, with two to three supervised sessions per week. Afterward, a maintenance plan keeps the gains.
Will my inhaler use change after rehab?
You’ll often learn a better inhaler technique, which can improve drug delivery. Some patients can reduce rescue inhaler reliance because they experience fewer flare‑ups.
Can I do the exercises at home?
Yes. After the initial supervised phase, most clinicians provide a home‑exercise booklet and video links. Consistency is key, so schedule short sessions daily.
Whether you’re newly diagnosed or have been living with asthma for years, incorporating pulmonary rehabilitation could be the game‑changer you’ve been waiting for. Talk to your doctor today and ask about a program that fits your lifestyle.


Poornima Ganesan
October 18, 2025 AT 14:19First, let me clarify that pulmonary rehabilitation is not a trendy side‑effect of pharma marketing, it is a rigorously studied multidisciplinary intervention that can genuinely improve asthma outcomes. The program combines aerobic conditioning, resistance work, and targeted breathing techniques, which together enhance diaphragmatic strength and reduce hyper‑responsiveness. Studies from 2022 to 2024 consistently show a double‑digit increase in FEV1, far beyond the modest gains seen with inhaler optimization alone. Moreover, the psychosocial component tackles the anxiety loop that keeps patients sedentary, which is often the hidden driver of deconditioning. By logging symptoms and spirometry results, clinicians can tailor intensity, preventing exacerbations during training. The education modules on inhaler technique also ensure that medication delivery is maximized, something many patients overlook. Community support groups foster peer accountability, turning solitary fear into collective empowerment. The incremental progression from low‑intensity walks to interval training mirrors the physiological adaptation curve, preventing plateau. Regular outcome monitoring with the six‑minute walk test provides objective proof that the body is responding positively. Importantly, the reduction in hospital admissions observed in longitudinal cohorts translates to real‑world cost savings for the healthcare system. Patients frequently report a newfound confidence that extends beyond the gym, influencing daily chores and even occupational performance. This confidence is not merely psychological; it reflects measurable improvements in muscle endurance and lung elasticity. The structured nature of the program also builds routine, which is essential for chronic disease management. In short, pulmonary rehabilitation addresses the root causes of asthma‑related disability rather than just the symptoms. If you are still skeptical, consider that the same principles that help COPD patients thrive are now being adapted with asthma‑specific nuances, creating a hybrid model that works for a broad spectrum of respiratory patients.
Brian Van Horne
November 5, 2025 AT 05:19The systematic inclusion of exercise, education, and psychosocial support within a monitored timeframe exemplifies best‑practice care for chronic respiratory disease.
Norman Adams
November 22, 2025 AT 21:19Oh sure, because adding a few weeks of treadmill time magically cures the complexities of asthma-next they'll tell us yoga cures heart disease.
Margaret pope
December 10, 2025 AT 13:19actually the rehab teams do a lot of work beyond just cardio they teach breathing tricks and give you tools to manage stress while you breathe easier
Linda A
December 28, 2025 AT 05:19In the quiet corridors of self‑reflection, we find that healing is less about the external regimen and more about the inner acceptance of our frailties.
Albert Fernàndez Chacón
January 14, 2026 AT 21:19I’ve been through a rehab program and the biggest win for me was actually learning how to use my inhaler correctly; the breathing drills felt weird at first but they helped me feel less out of breath when climbing stairs.
Drew Waggoner
February 1, 2026 AT 13:19Great info, thanks.
Mike Hamilton
February 19, 2026 AT 05:19i think its super interessting how thoery from physiotherpay and lung med get blended in these progreams it shows that health is not just a single displin it’s a whole ecosystem of care