Drug Labeling Differences: Why Packaging and Warnings Vary Across Countries
When you pick up a pill bottle, the text on the label isn’t just random info—it’s a drug labeling, the official printed information on a medication’s packaging that tells users how to take it, what risks to watch for, and who it’s meant for. Also known as medication labeling, it’s designed to protect you, but it’s not the same everywhere. In the U.S., the FDA labeling, the set of rules and formats the U.S. Food and Drug Administration requires for prescription and OTC drug packaging is strict about black box warnings, dosage charts, and side effect lists. But in Canada, Health Canada labeling, the national standard for how drugs are labeled in Canada, including language requirements and risk communication often includes more plain-language summaries and bigger fonts for older adults. Even the same drug made by the same company can have different labels depending on where it’s sold.
Why does this matter? Because small differences in wording can change how you use the medicine. A label in the U.S. might say "take with food" in small print, while the Canadian version puts it in bold at the top. One country might list dizziness as a "common" side effect; another calls it "rare." Some labels include photos of the pill, others don’t. Some list drug interactions in a chart; others bury them in paragraphs. These aren’t just design choices—they’re legal and cultural decisions. The FDA focuses on detailed clinical data, while Health Canada and the EMA in Europe often prioritize patient comprehension. That’s why someone buying generic amoxicillin or tetracycline online might get a bottle with a label they’ve never seen before. It’s not a fake—it’s just labeled for a different market.
These differences show up in real ways. A patient switching from a U.S. prescription to a Canadian one might miss a warning about driving because the alert was moved. An older adult might misread a dose because the font size changed. Even the color of the pill bottle or the shape of the warning symbol can confuse people who rely on visual cues. That’s why checking the label every time—even for a drug you’ve taken before—isn’t just smart, it’s necessary. The drug labeling differences you see aren’t random. They’re shaped by regulators, language laws, and how each country thinks patients should be informed. Below, you’ll find real stories and guides on how these differences impact safety, perception, and outcomes—from how generic drugs are labeled to why some warnings get ignored. These aren’t just technical details. They’re life-changing details.
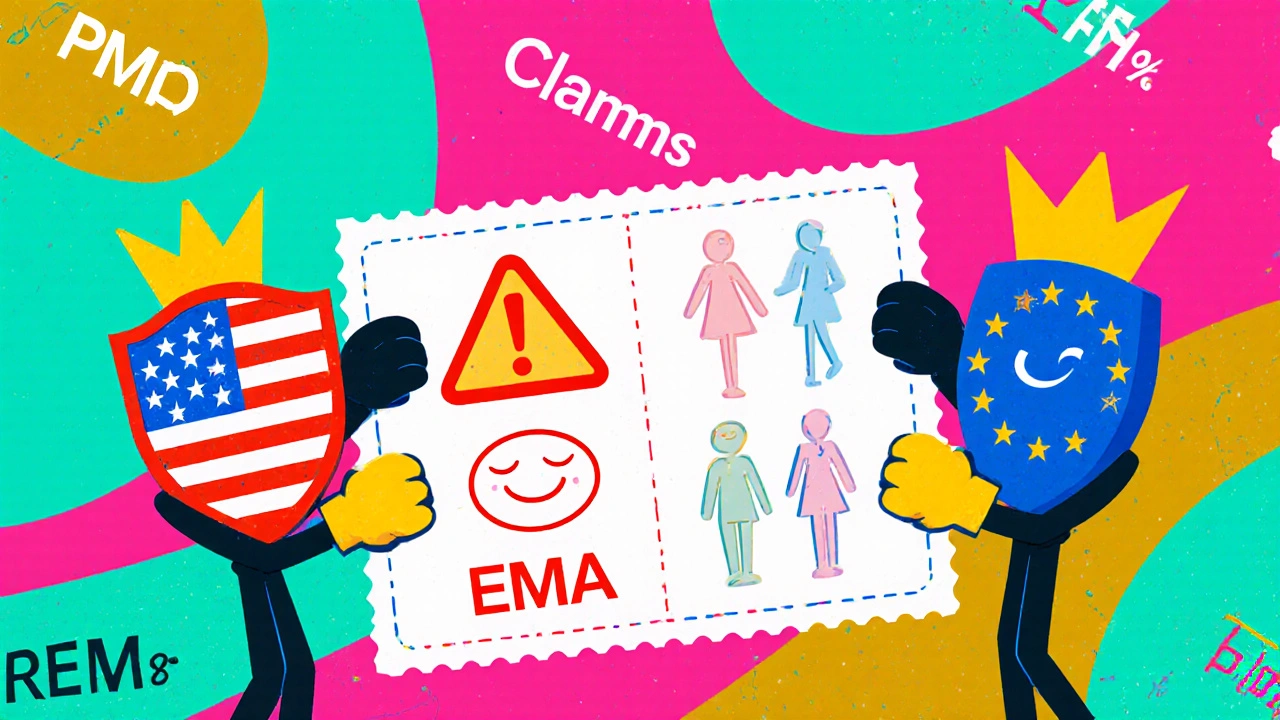
EMA vs FDA Drug Labeling: Key International Differences That Impact Global Drug Access
EMA and FDA drug labeling differ significantly in scope, language, risk communication, and approval standards. Understanding these differences is critical for global healthcare providers and pharmaceutical companies.