Understanding Stent Thrombosis Risk
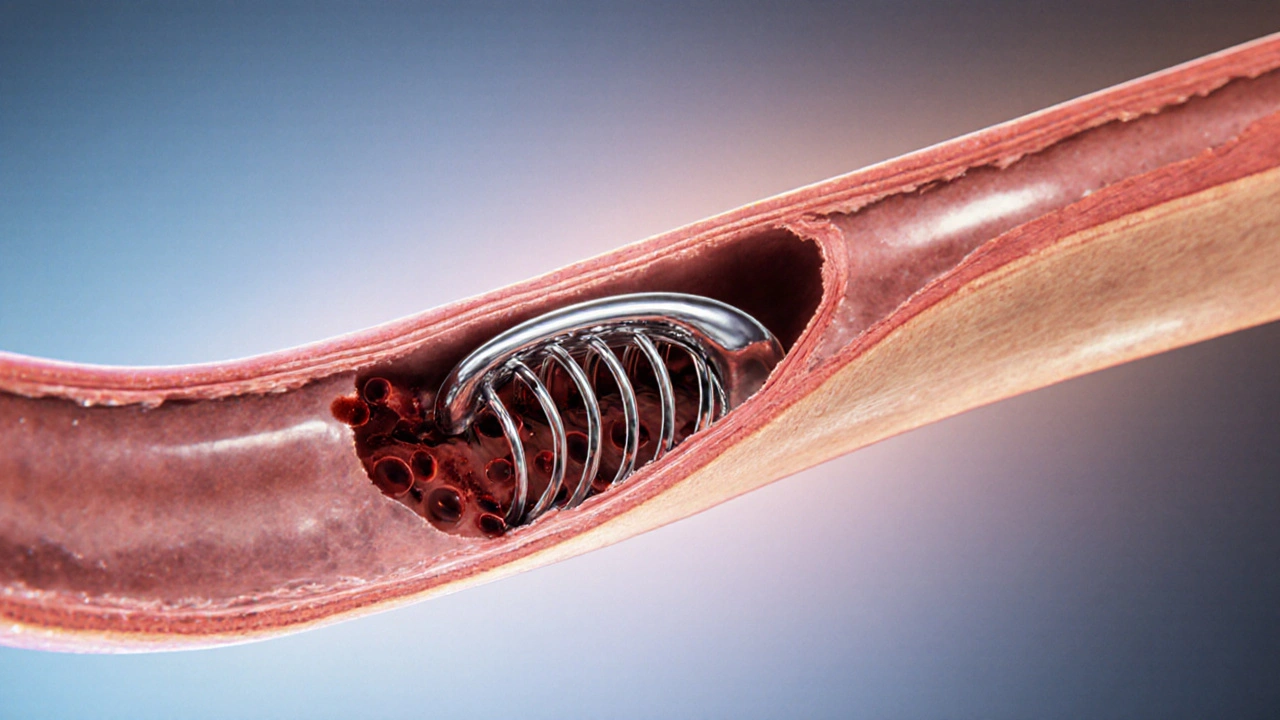
When dealing with stent thrombosis risk, the chance that a blood clot forms inside a coronary stent after a heart procedure. Also known as clot risk in stented arteries, it is a critical concern for anyone who has undergone a percutaneous coronary intervention, a minimally invasive technique to open blocked heart vessels. A coronary stent, a tiny mesh tube that props open a narrowed artery can be either a drug‑eluting stent, which releases medication to prevent tissue growth or a bare‑metal version. The type of stent you receive directly influences the clot‑forming potential, making the choice of dual antiplatelet therapy, a combination of aspirin and a P2Y12 inhibitor taken after the procedure a cornerstone of risk management. In short, stent thrombosis risk encompasses clot formation inside the stent, requires antiplatelet medication, and is shaped by the device and the procedure itself.
Key Contributors and How They Interact
First, the stent’s design matters. Drug‑eluting stents lower the chance of tissue overgrowth, but some early‑generation models were linked to higher late‑stage clot rates, prompting newer alloys and polymer coatings. Second, the timing and adherence to dual antiplatelet therapy is a make‑or‑break factor; stopping the meds too early can spike clot risk, while prolonged use raises bleeding concerns. Third, patient‑specific issues such as diabetes, smoking, or high cholesterol act as amplifiers, nudging the risk curve upward. Finally, the procedural technique—proper sizing, adequate lesion preparation, and optimal deployment pressure—helps ensure the stent sits flush against the vessel wall, reducing turbulent flow that can trigger clot formation. Each of these elements sits in a cause‑effect chain: a well‑chosen stent plus precise implantation plus consistent medication equals a lower probability of thrombosis.
Understanding these links empowers you to ask the right questions at your cardiologist’s office. You might inquire about the latest‑generation drug‑eluting stent, confirm the recommended duration of dual antiplatelet therapy, and discuss lifestyle tweaks that cut the odds of clotting. You can also request follow‑up imaging, such as a coronary CT angiogram, to verify that the stent remains open and unthrombosed. By treating stent thrombosis risk as a multi‑factor puzzle rather than a single event, you gain a clearer roadmap to a safer heart after the procedure.
Below you’ll find articles that dive deeper into medication choices, procedural techniques, and patient monitoring so you can manage stent thrombosis risk with confidence and clarity.
How Exercise Helps Prevent Blood Clots in Stents
Learn how regular exercise lowers the risk of blood clots in coronary stents, what types of activity work best, and how to combine workouts with medication safely.