When you start treatment for osteoporosis, you don’t have to wait two years to know if it’s working. That’s the game-changing truth behind bone turnover markers. These aren’t fancy lab jargon-they’re real, measurable signals from your bones that tell your doctor whether your medication is actually doing its job. And they do it in weeks, not years.
What Are Bone Turnover Markers?
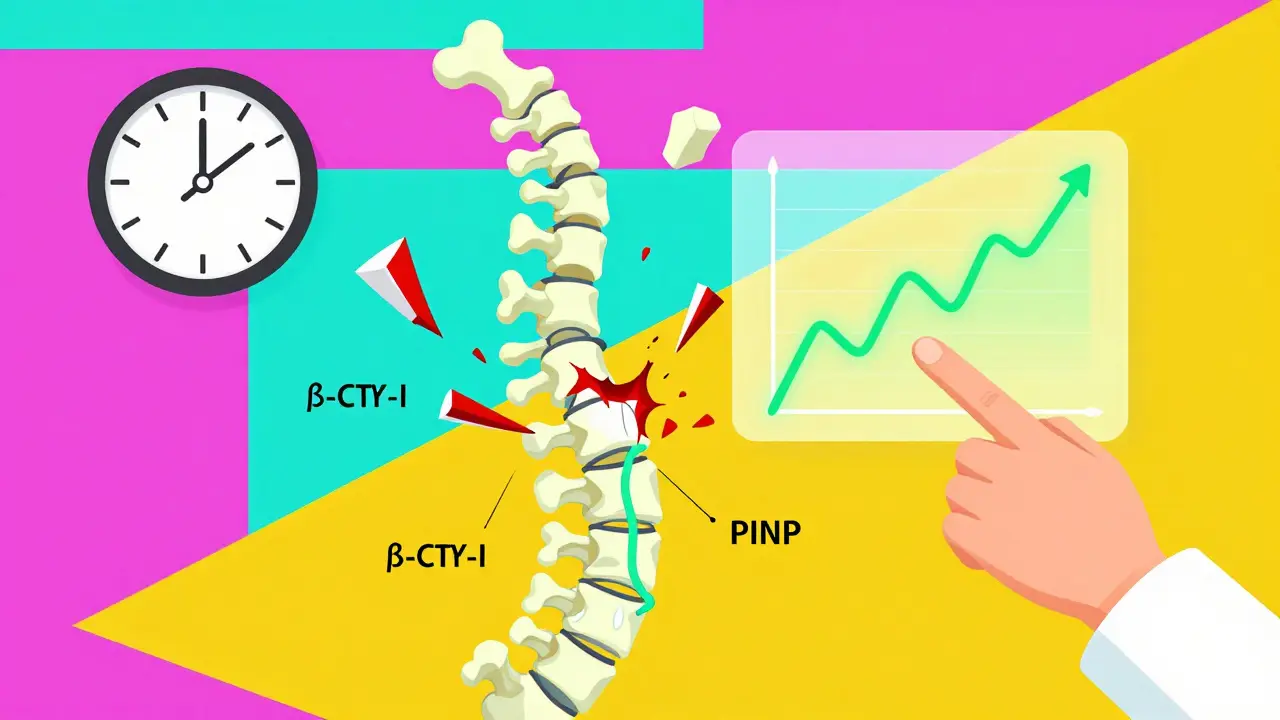
Your bones are never still. Even when you’re sitting still, they’re constantly being broken down and rebuilt. This process is called bone remodeling. When you have osteoporosis, that balance is off-your body breaks down bone faster than it rebuilds it. That’s where bone turnover markers (BTMs) come in. They’re tiny protein fragments and enzymes released into your blood or urine when bone is being formed or broken down. There are two main types:- Formation markers: Show new bone being made. The most reliable is PINP (procollagen type I N-terminal propeptide).
- Resorption markers: Show bone being broken down. The gold standard here is β-CTX-I (beta C-terminal telopeptide of type I collagen).
Why Wait Two Years When You Can Know in Three Months?
Most people think the only way to track osteoporosis treatment is with a bone density scan (DEXA). But here’s the problem: DEXA scans change slowly. Even if your medication is working perfectly, it takes 12 to 24 months to see a measurable increase in bone density. That’s a long time to wonder if you’re wasting your time-or worse, if you’re still at risk for fractures. Bone turnover markers change fast. Within 3 to 6 weeks of starting a drug like alendronate or denosumab, your β-CTX-I levels will drop. If you’re on teriparatide (an anabolic drug), your PINP levels will jump. That’s not noise-that’s your bones responding. A 2022 study called TRIO showed patients who had a 30% or greater drop in β-CTX-I after 3 months had a 1.6% lower fracture risk over the next 22 weeks. That’s not a small win. That’s a life-changing difference.Which Markers Are Actually Used in Real Clinics?
Not all bone markers are created equal. Back in the 2000s, doctors tested a dozen different ones. Now, thanks to global consensus from the International Osteoporosis Foundation and European Calcified Tissue Society, we know exactly which two to trust:- PINP (serum): Best for tracking bone formation. Stable, reliable, low biological variation.
- β-CTX-I (plasma): Best for tracking bone breakdown. Highly sensitive to treatment changes.
How Do You Actually Get Tested?
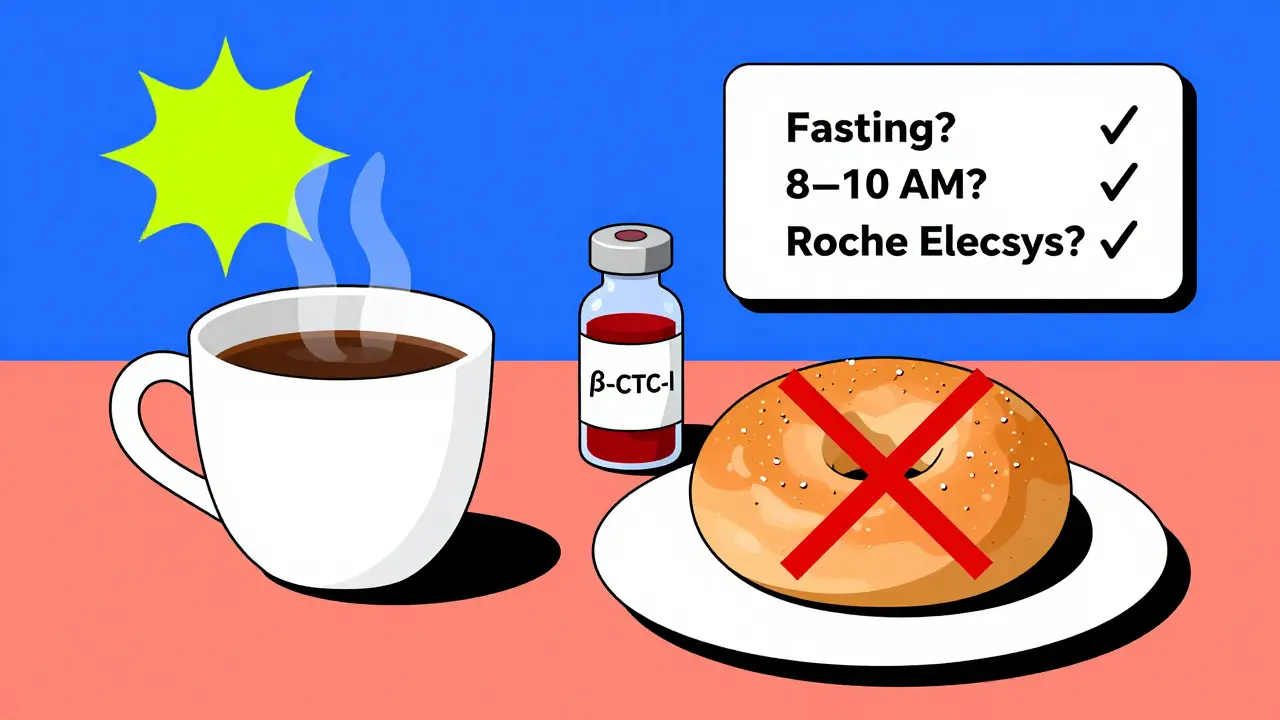
It sounds simple, but the devil’s in the details. If you don’t follow the rules, your results are useless. For β-CTX-I:- Fast overnight-no food or drink except water.
- Draw blood between 8 and 10 a.m.
- Don’t eat or drink anything for 2 hours before the test.
- Fasting is still preferred, but less critical.
- Still best to collect in the morning.
- Diurnal variation is only 10-15%, so it’s more forgiving.
What Do the Numbers Mean?
A single number doesn’t mean much. What matters is the change from your baseline. For antiresorptive drugs (like bisphosphonates or denosumab):- Good response: More than 30% drop in β-CTX-I.
- Good response: More than 35% rise in PINP? No-wait. That’s wrong. PINP goes up with anabolic drugs, not down with antiresorptives. For antiresorptives, PINP drops by 30-50%.
- Good response: PINP increases by 70-100% within 1-3 months.
- β-CTX-I may rise slightly, but PINP is the star here.
When Should You Get Tested?
There’s a clear, evidence-based timeline:- Before starting treatment: Get your baseline PINP and β-CTX-I. This is non-negotiable.
- At 3 months: Repeat the test. This tells you if your body is responding.
- At 6 months: Optional, but helpful if the 3-month result was borderline.
- At 12-24 months: DEXA scan. This is still the gold standard for confirming long-term bone density gains.
Who Should Get Tested-and Who Shouldn’t?
This isn’t for everyone. But it’s critical for certain people:- Those starting antiresorptive or anabolic therapy.
- Patients who miss doses or complain of side effects.
- People with kidney disease-where standard markers can be misleading.
- Anyone with a high fracture risk and no clear response to treatment.
- Postmenopausal women without osteoporosis (yet).
- People on calcium or vitamin D alone.
- Those who’ve already had a DEXA scan showing stable bone density and no symptoms.
Why Isn’t Everyone Using This?
You’d think every doctor would jump on this. After all, it’s cheaper than a DEXA scan, less radiation, and faster. But here’s the truth: adoption is still low. In Europe, 45-60% of clinics use BTMs regularly. In the U.S.? Only 25-35%. Why? Three reasons:- Doctors don’t know how to interpret them. A 2023 IOF survey found most primary care providers need 2-4 hours of training just to feel confident.
- Lab variability. Only 65% of U.S. labs follow the IFCC’s standardized protocols.
- Insurance confusion. Medicare covers PINP (CPT 83970) and β-CTX-I (CPT 83935), but many private insurers still treat them as “experimental.”
The Bottom Line: It’s Not Either/Or
Bone turnover markers don’t replace DEXA scans. They complement them. Think of it this way: DEXA tells you how strong your bones are right now. BTMs tell you whether your treatment is making them stronger-or not. If you’re on osteoporosis meds, ask your doctor:- “Have I had a baseline PINP and β-CTX-I test?”
- “When should I get them repeated?”
- “What’s my target reduction or increase?”
It’s not magic. It’s science. And it’s here.
What are the best bone turnover markers for monitoring osteoporosis treatment?
The two most reliable bone turnover markers are serum PINP (procollagen type I N-terminal propeptide) for bone formation and plasma β-CTX-I (beta C-terminal telopeptide of type I collagen) for bone resorption. These are endorsed by the International Osteoporosis Foundation and European Calcified Tissue Society as the global reference standards. Other markers like osteocalcin or urinary NTx are no longer recommended due to higher variability and lack of standardization.
How soon can I see results from bone turnover marker testing after starting treatment?
Changes in bone turnover markers appear within 3 to 6 weeks of starting osteoporosis treatment. For antiresorptive drugs like bisphosphonates, β-CTX-I levels drop significantly by 3 months. For anabolic drugs like teriparatide, PINP levels rise sharply within 1 to 3 months. This is much faster than DEXA scans, which require 12 to 24 months to detect meaningful changes in bone density.
Do I need to fast before a bone turnover marker test?
Yes-for β-CTX-I, fasting overnight is required. You should also avoid eating or drinking anything except water for at least 2 hours before the test. Blood should be drawn between 8 and 10 a.m. to account for natural daily fluctuations. PINP is less affected by food, but fasting and morning collection are still recommended for consistency. Skipping these steps can make your results inaccurate by up to 40%.
What if my bone turnover marker results don’t change after 3 months?
If your β-CTX-I doesn’t drop by at least 30% (or your PINP doesn’t rise by 70-100% on anabolic therapy), it could mean you’re not taking your medication as prescribed, your body isn’t responding, or you have an underlying condition like kidney disease. Your doctor may check your adherence, adjust your dose, switch medications, or investigate other causes. Non-response is a red flag that needs action-not just waiting.
Can bone turnover markers predict fracture risk?
Yes. Multiple studies, including the TRIO trial, show that patients who achieve a 30% or greater reduction in β-CTX-I within 3 months have a significantly lower fracture risk over the next year compared to non-responders. While DEXA scans measure bone density, BTMs measure bone activity-making them powerful predictors of treatment effectiveness and future fracture risk, especially when used together.
Are bone turnover markers covered by insurance?
In the U.S., Medicare covers both PINP (CPT code 83970) and β-CTX-I (CPT code 83935) for osteoporosis monitoring. Reimbursement rates are around $28-$33 per test. Many private insurers now cover them too, especially if ordered by an endocrinologist or rheumatologist. However, some still require prior authorization. Always check with your insurer before testing.
Do bone turnover markers work the same for all ethnic groups?
No. Baseline levels vary by ethnicity. Asian populations tend to have 15-20% lower β-CTX-I levels than Caucasians. African populations often show 10-15% higher PINP levels. Most reference ranges were developed using Caucasian data, so results may need adjustment based on your background. Clinicians should consider ethnicity when interpreting results, and labs are urged to expand reference studies to include more diverse populations.
Can I use bone turnover markers if I have kidney disease?
Standard markers like PINP and β-CTX-I can be falsely elevated in chronic kidney disease because the kidneys can’t clear them from the blood. In these cases, bone alkaline phosphatase (BALP), intact PINP, or TRACP5b are better alternatives. These markers are less affected by kidney function. If you have CKD, ask your doctor to order these specific markers instead-and make sure the lab uses reference ranges adjusted for your kidney stage.





Kiran Plaha
January 5, 2026 AT 18:52This is actually super helpful. I’ve been on alendronate for 6 months and my doctor never mentioned these tests. I had no idea you could tell if it’s working this fast.
Matt Beck
January 6, 2026 AT 09:38So… you’re telling me my bones are having a little party every time I take my pill? 🎉💥 PINP up = bone babies! β-CTX-I down = no more bone carnage! Science is wild. I feel like my skeleton just gave me a high-five.
Beth Templeton
January 7, 2026 AT 19:49Wow. A whole article about two blood tests. And you made it sound like a miracle. Congrats.
Tiffany Adjei - Opong
January 9, 2026 AT 15:06Okay but let’s be real - if your doctor doesn’t even know how to interpret these, why are we supposed to care? I’ve had three different labs give me three different β-CTX numbers. One said I was ‘responding,’ another said ‘borderline,’ and the third said ‘your coffee ruined everything.’
Also, PINP is 70% more expensive than a DEXA. Who’s paying for this? Not Medicare, not my insurance, not my wallet.
And don’t get me started on ‘ethnic adjustments.’ So now I’m not just osteoporotic, I’m ethnically osteoporotic? Great.
Ryan Barr
January 10, 2026 AT 14:39Only two markers? How quaint. In my PhD thesis, we used 17 biomarkers with LC-MS/MS and Bayesian modeling. This is basic clinical hygiene.
Cam Jane
January 12, 2026 AT 10:45Y’ALL. I just got my 3-month BTM results and my β-CTX dropped 42%! I cried. Not because I’m emotional - because I’ve been taking my meds every single day for a year and no one ever told me I’d see proof this fast. My doctor just shrugged before. Now she’s printing out the paper. You’re not just getting tested - you’re getting empowered. Tell your mom. Tell your aunt. Tell your neighbor who’s scared of falling. This isn’t just science - it’s hope in a vial.
Dana Termini
January 14, 2026 AT 07:24I appreciate the clarity here. I’ve been skeptical of biomarkers because I’ve seen too many overhyped trends. But this feels grounded. The fasting rules, the lab standards, the LSC thresholds - it’s all very methodical. I’m going to ask my endo for the tests next visit.
Amy Le
January 15, 2026 AT 15:49USA is falling behind again. In Germany, this is standard. In Japan, they use it to adjust doses monthly. We’re still arguing about whether to call it ‘bone turnover’ or ‘bone remodeling.’ 🇺🇸
Also, why does every American article sound like a TED Talk? ‘It’s not magic. It’s science.’ No, it’s a blood draw and a spreadsheet.
Stuart Shield
January 15, 2026 AT 21:51Man, I remember when we used to just guess if bisphosphonates were working. I used to tell patients, ‘Come back in two years, we’ll see.’ Now? We’ve got this beautiful little window into what’s happening inside their bones. It’s like having X-ray vision for healing. And yeah, the fasting is annoying - but it’s worth it. Don’t skip the coffee rule. Your bones will thank you.
Lily Lilyy
January 17, 2026 AT 19:57Thank you for sharing this with such care and precision. It is a gift to have access to such clear, evidence-based guidance. I will share this with my community center’s senior wellness group. Knowledge is power, and you have given us a powerful tool to advocate for ourselves.
Katelyn Slack
January 18, 2026 AT 13:31wait so you mean i dont have to wait 2 years?? i thought i was just supposed to take my pill and hope??