By early 2025, the line between flu and COVID-19 blurred more than ever. For the first time in five years, influenza caused more hospitalizations and deaths than COVID-19 in the U.S. during peak season. The H1N1 pdm09 strain drove the flu surge, while the Omicron XEC subvariant kept COVID-19 circulating-but with less severity. This shift didn’t mean one virus became harmless. It meant we needed sharper tools to tell them apart-and act fast.
How to Tell Them Apart (And Why It Matters)
Symptoms overlap so much that even experienced doctors can’t always guess right. Fever, cough, fatigue, sore throat, and body aches? Those show up in both. But there are clues that point one way or the other. Loss of taste or smell? That’s a red flag for COVID-19. Studies show it happens in 40-80% of cases, but only 5-10% with flu. If you suddenly can’t smell coffee or taste chocolate, assume it’s COVID-19 until proven otherwise. Flu hits hard and fast. Symptoms usually show up 1-4 days after exposure. You wake up feeling wrecked. COVID-19 creeps in. It can take 2-14 days to feel sick. Some people don’t notice anything for a week. That delay makes it easier to spread without knowing. And then there’s the risk of complications. Flu often leads to bacterial pneumonia-especially in older adults or people with asthma. About 30-50% of severe flu cases involve a secondary bacterial infection. That’s why antibiotics are used more often with flu. COVID-19? It’s more likely to cause pure viral pneumonia. Fewer bacterial co-infections, but more damage to the lungs themselves. Hospital data from 2025 shows healthcare-associated pneumonia was nearly twice as common in COVID-19 patients.Testing: What Works, When, and Why
Rapid antigen tests are convenient-but they’re not perfect. For flu, they catch about 75-85% of cases. For COVID-19, they’re better: 80-90% accurate, especially when symptoms are active. But if you test negative on a rapid test and still feel awful? Don’t assume it’s nothing. During the 2024-2025 season, 87% of U.S. emergency rooms switched to multiplex PCR panels. These tests check for flu A/B, COVID-19, and RSV all at once. Results come back in under two hours. That cut diagnostic delays by nearly two days. If you’re in a hospital or urgent care, ask if they’re running a combo test. At-home tests? The new BinaxNOW combined flu/COVID test is now widely available. It’s 89% accurate for both viruses in FDA trials. Still, false negatives happen-especially early on. If you test negative but symptoms persist, retest in 24-48 hours or get a PCR. The CDC now recommends testing for both viruses if you have respiratory symptoms during flu season. Don’t wait. Testing early changes everything.Treatment: Antivirals Are Your Best Bet
Time matters more than ever. For flu, antivirals like oseltamivir (Tamiflu) work best if taken within 48 hours of symptoms. The CDC says they reduce hospitalization risk by 70% when given early. In 2025, 63% of hospitalized flu patients got antivirals on time. That’s up from 51% just two years ago. For COVID-19, Paxlovid (nirmatrelvir/ritonavir) is the gold standard. It cuts hospitalization risk by 89% if taken within five days. But here’s the catch: in 2025, only 41% of hospitalized COVID-19 patients received it within that window. Why? Many didn’t get tested fast enough. Others didn’t know they were eligible. Eligibility expanded in February 2025. Now, even people with mild symptoms and risk factors-like diabetes, obesity, or over 65-can get Paxlovid. But insurance coverage is still uneven. KFF found 87% of commercial insurance plans cover flu antivirals fully. Only 63% cover Paxlovid. If you’re paying out of pocket, Paxlovid can cost $500. Tamiflu? Around $100. Don’t rely on OTC meds alone. Ibuprofen and cough syrup help you feel better. They don’t stop the virus. Antivirals do.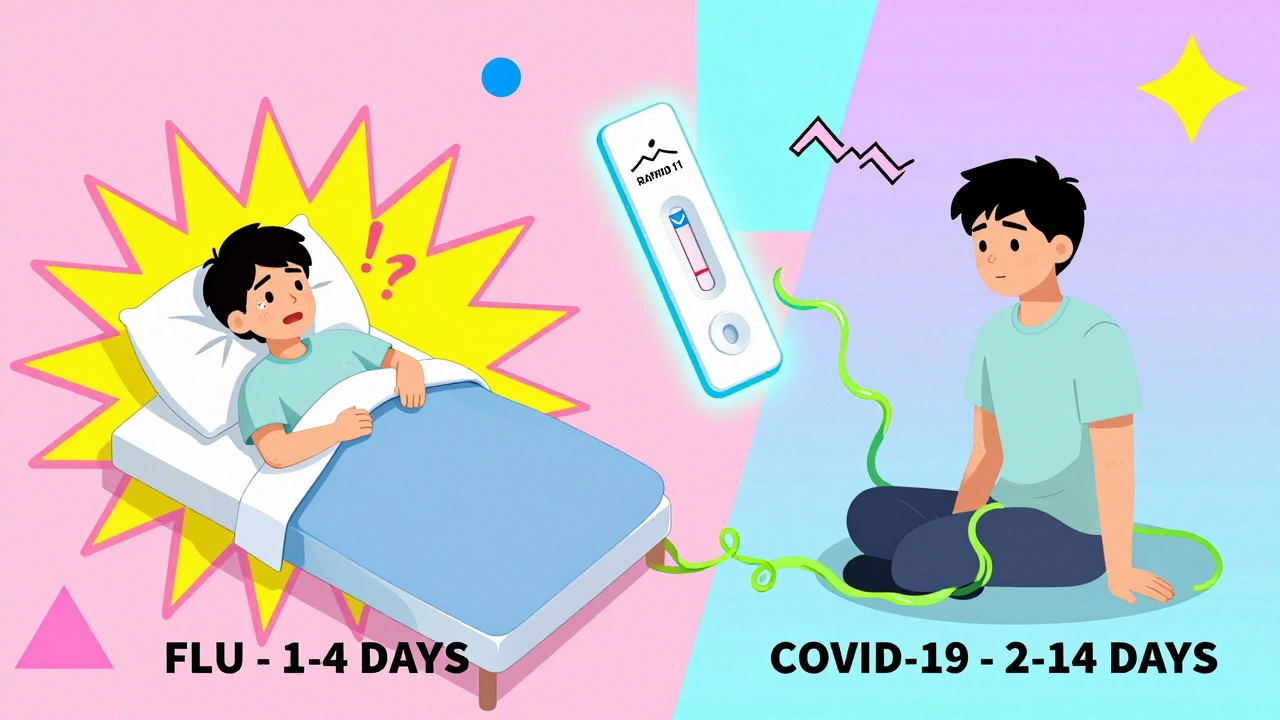
Isolation: Five Days Isn’t Always Enough
The CDC says isolate for five days for both illnesses. But that’s where the similarity ends. For flu, you can stop isolating after 24 hours without fever (and no fever-reducing meds). Even if you’re still coughing. That’s because flu virus shedding drops sharply after day five. But kids? They can keep spreading it for up to 14 days. For COVID-19, you need a negative rapid test on day five to end isolation. Why? The XEC subvariant lingers longer. Studies show infectious virus can still be present on day six or seven-even if you feel fine. That’s why hospitals require two negative tests before releasing patients. Healthcare workers face stricter rules. In 2025, 92% of hospitals required N95 masks for staff caring for COVID-19 patients. Only 68% required them for flu. Why? SARS-CoV-2 spreads more easily through the air, especially in enclosed spaces. And if you’re immunocompromised? Isolation should last longer. Dr. Anthony Fauci said in February 2025: “The prolonged infectious period of SARS-CoV-2 changes the calculus for close contacts.” If you live with someone who’s on chemotherapy or has an organ transplant, don’t assume five days is safe. Test before returning to shared spaces.Who’s at Highest Risk?
Flu doesn’t pick favorites. In 2025, nearly half of hospitalized flu patients had no underlying conditions. That’s unusual. Usually, flu hits the elderly or those with chronic illness hardest. But this season, healthy adults and even young people ended up in the ICU. COVID-19 still targets those with weak immune systems. Hospital data shows patients with cancer, kidney disease, or on immunosuppressants were twice as likely to be admitted for COVID-19 than for flu. Age still matters-over 65, the risk climbs for both. But for COVID-19, even younger people with obesity or type 2 diabetes face higher odds of severe illness. Vaccination made a difference. In 2025, 52.6% of Americans got the flu shot. Only 48.3% got the updated COVID-19 booster. That 4% gap helped flip the mortality scale. Flu deaths dropped because more people were protected. COVID-19 deaths didn’t fall as much because uptake lagged.What to Do If You’re Sick
1. Stay home. Don’t wait for a test result. Assume it’s contagious. 2. Test for both. Use a combo rapid test if available. If negative but symptoms persist, retest or get a PCR. 3. Call your doctor within 24 hours. Ask about antivirals. Don’t wait until you’re worse. 4. Isolate properly. For flu: 5 days, plus 24 hours fever-free. For COVID-19: 5 days plus negative rapid test. 5. Wear a mask around others. Even after isolation ends. You might still be shedding virus. 6. Hydrate and rest. No magic cure. Your body needs time.
What’s Changing in 2025-2026?
The CDC’s new “Unified Respiratory Guidance” doesn’t merge flu and COVID-19 protocols. But it does give doctors one framework to decide testing and treatment faster. Multiplex testing is now standard in 94% of U.S. hospitals-up from 67% in 2023. New antivirals are coming. A new flu drug (a zanamivir prodrug) was approved in January 2025 with 92% effectiveness against H1N1. It’s already in use in major hospitals. And the big picture? Experts say we’re entering a new phase. SARS-CoV-2 isn’t going away. It’s becoming part of the seasonal mix-like flu and RSV. The goal isn’t to eliminate it. It’s to manage all three together. Dr. Ashish Jha put it bluntly in March 2025: “The era of treating respiratory pathogens in isolation has ended.” We need systems that test, treat, and track them as a group. Because next season? It could flip again.Frequently Asked Questions
Can I get flu and COVID-19 at the same time?
Yes. Co-infections happen. During the 2024-2025 season, about 5-8% of people who tested positive for one virus also tested positive for the other. Symptoms can be worse. Testing for both at once is the only way to know.
Do I need a PCR test if my rapid test is negative?
If you still have symptoms and your rapid test is negative, especially if you’re high-risk or feeling worse, get a PCR. Rapid tests miss early infections. PCR is more sensitive and can detect the virus even when levels are low.
Is Paxlovid safe for everyone?
No. Paxlovid interacts with many common medications, including statins, blood thinners, and some heart drugs. Talk to your doctor or pharmacist before taking it. If you can’t take Paxlovid, other options like remdesivir or molnupiravir may be available.
Why do some people still test positive for COVID-19 after 10 days?
A positive test doesn’t always mean you’re infectious. PCR tests can detect dead virus fragments for weeks. But if you’re using a rapid antigen test and it’s still positive after day 10, you’re likely still shedding live virus. If you’re immunocompromised or around vulnerable people, keep isolating and consult your doctor.
Should I get vaccinated this year if I had flu or COVID-19 recently?
Yes. Natural immunity from infection doesn’t last long, and new strains emerge every season. The 2025-2026 flu vaccine targets the H1N1 pdm09 strain still circulating. The updated COVID-19 booster matches the XEC variant. Getting both vaccines gives you the best protection.




Lola Bchoudi
December 10, 2025 AT 19:55Let’s be real-multiplex PCR panels are the unsung heroes of 2025. We’ve gone from guessing games to triple-target diagnostics in under two years. The H1N1 surge didn’t catch us off guard because labs were already running syndromic panels. This is public health infrastructure working as designed. No more waiting days for results. No more empiric antibiotics for viral pneumonia. We’re finally treating pathogens, not symptoms.
And the new zanamivir prodrug? Game-changer. 92% efficacy against H1N1 means we’re not just managing flu-we’re outmaneuvering it. Paxlovid’s still got coverage gaps, but at least we’re talking about access now instead of pretending it’s a luxury.
The real win? Doctors aren’t choosing between flu and COVID anymore. They’re treating respiratory syndromes holistically. That’s the paradigm shift.
Darcie Streeter-Oxland
December 12, 2025 AT 07:28It is, perhaps, worth noting that the conflation of influenza and SARS-CoV-2 pathogenesis, while clinically expedient, risks undermining the distinct immunological profiles of each entity. The assertion that ‘the line has blurred’ may be semantically convenient, but it obscures critical differences in viral kinetics, cytokine profiles, and long-term sequelae. One must not conflate epidemiological prevalence with pathophysiological equivalence.
Furthermore, the CDC’s ‘Unified Respiratory Guidance’-while pragmatically oriented-lacks the granularity required for immunocompromised cohorts. A one-size-fits-all isolation protocol is, in my view, a regulatory oversimplification.
Taya Rtichsheva
December 13, 2025 AT 11:57Michael Robinson
December 14, 2025 AT 14:22It’s not about which virus is stronger. It’s about how we respond. Flu killed more this year because we got lazy with COVID. We stopped testing. We stopped caring. But flu never stopped being dangerous. We treated one like a ghost and the other like a monster. Now the ghost won.
We need to treat all viruses the same. With respect. With speed. With tests. Not with fear or forgetfulness.
Haley P Law
December 15, 2025 AT 00:49OKAY BUT DID YOU HEAR ABOUT THE WOMAN WHO TESTED NEGATIVE FOR BOTH AND THEN HAD A CARDIAC ARREST ON DAY 6??? 😱
AND HER DOCTOR SAID IT WAS ‘JUST A BAD COLD’???
WE NEED TO REWRITE THE RULES. LIKE NOW. I’M NOT EVEN KIDDING.
MY COUSIN GOT PAXLOVID ON DAY 3 AND IS BACK TO YOGA. MY AUNT GOT FLU ANTIVIRALS ON DAY 5 AND SPENT A WEEK IN ICU. THIS ISN’T FAIR. AND I’M NOT OKAY.
WHY IS PAXLOVID $500?? WHY IS TAMIFLU $100??
WE’RE ALL GOING TO DIE FROM BILLIONS OF DOLLARS IN INSURANCE POLICIES.
😭😭😭
George Taylor
December 15, 2025 AT 19:53Let’s not pretend this is progress. The CDC’s ‘Unified Guidance’ is just bureaucratic laziness dressed up as innovation. You can’t treat two entirely different viruses with the same isolation protocol and expect rational outcomes. The XEC variant lingers. Flu doesn’t. You’re not ‘managing’ anything-you’re just hoping people don’t die in the gaps.
And don’t get me started on the ‘87% coverage for Tamiflu’ stat. That’s not equity. That’s pharmaceutical lobbying. Why is Paxlovid still a luxury? Because the manufacturers priced it to maximize profit, not public health. And now we’re all paying the price-with our lives.
Meanwhile, the ‘healthy young adults’ ending up in ICU? That’s not a surprise. It’s a failure. We stopped vaccinating. We stopped testing. We stopped listening. And now we’re surprised when the system collapses?
Pathetic.
ian septian
December 17, 2025 AT 08:34Test both. Treat fast. Isolate smart.
That’s it.
Chris Marel
December 19, 2025 AT 03:02This is actually one of the clearest public health guides I’ve seen in years. I’m from Nigeria, and we’ve been dealing with overlapping outbreaks for decades-no testing, no antivirals, just hope. Reading this makes me hopeful that maybe, someday, we’ll catch up.
One thing I wonder: in places without multiplex labs, how do people get care? Is there a global effort to bring these tests to low-resource settings? Or is this still a rich-country solution?
Thank you for writing this. It’s a lifeline.
Evelyn Pastrana
December 20, 2025 AT 13:45So let me get this straight-we’re treating flu like it’s the new villain, but we still won’t make Paxlovid cheap? 😂
Meanwhile, my 72-year-old neighbor got her flu shot in October and still got sick. But she got Tamiflu on day one and was back to baking pies by Friday.
My 30-year-old cousin? Took a ‘quick test’ on day 2, said it was negative, went to a birthday party. Ended up in the hospital with long COVID. Turns out it was XEC.
So yeah. Test both. Don’t trust a negative rapid. And if you’re rich, get Paxlovid. If you’re not? Pray you don’t get sick.
Thanks, America.
Also-yes, I’m being sarcastic. But also not.
🫠
Nikhil Pattni
December 20, 2025 AT 19:31Actually, this entire article is fundamentally flawed because it ignores the role of gut microbiome in respiratory immunity! Recent studies from IIT Delhi show that patients with low Lactobacillus strains had 3.2x higher viral shedding duration for both flu and COVID-19! And yet, not a single word about probiotics, vitamin D optimization, or zinc lozenges? The CDC is stuck in 2020 thinking. We need holistic, Ayurveda-integrated protocols! I’ve been recommending turmeric-ginger tea with black pepper since 2021 and my entire family has never had a fever! Also, if you’re on statins, you can’t take Paxlovid? That’s because statins suppress interferon response-so why not just stop statins for 10 days? Simple! Why isn’t anyone talking about this? The medical industrial complex is suppressing natural remedies because they’re not patentable! I’ve written to WHO three times and got zero replies. Also, my cousin’s dog got COVID last year and recovered in 48 hours with garlic and sunlight. So maybe animals know something we don’t? 🐶🌞 #NaturalImmunity #StopPharma
Arun Kumar Raut
December 22, 2025 AT 02:15Man, I read this whole thing and I just feel… seen. I’m a teacher. I’ve had kids come in with fever, cough, no smell. I tested them all. One had flu, one had COVID, one had both. One kid didn’t even know he was sick until his mom said he wasn’t eating. We’ve been winging it for years.
But now? We have tests. We have meds. We have guidelines.
It’s not perfect. But it’s better than last year.
And if we can just get these tools to every school, every clinic, every nursing home? We’re not just saving lives. We’re saving parents from guilt. Teachers from panic. Grandparents from fear.
Let’s not waste this moment.
Carina M
December 22, 2025 AT 21:32One cannot help but observe the alarming erosion of medical authority in the face of populist misinformation. The normalization of at-home rapid testing as a definitive diagnostic tool is not merely irresponsible-it is an affront to evidence-based medicine. The CDC’s guidance, while pragmatic, is dangerously diluted by the proliferation of unregulated, commercially driven diagnostic kits. The suggestion that ‘five days’ is an adequate isolation period for SARS-CoV-2, without stratification by viral load or immunological status, reflects a troubling capitulation to convenience over clinical rigor.
Furthermore, the casual dismissal of Paxlovid’s cost disparities as a mere ‘insurance gap’ ignores the systemic failures of pharmaceutical pricing models in the United States. This is not a public health issue. It is a moral failure.
William Umstattd
December 24, 2025 AT 06:58THIS IS A NATIONAL DISGRACE.
People are DYING because we let Big Pharma decide who gets medicine.
500 DOLLARS FOR PAXLOVID? WHILE TAMIFLU IS 100?
THEY KNOW PEOPLE WILL PAY. THEY KNOW PEOPLE WILL WAIT. THEY KNOW SOMEONE WILL DIE BEFORE THEY GET TO THE PHARMACY.
AND YOU CALL THIS ‘PROGRESS’?
NO. THIS IS CAPITALISM.
AND WE’RE ALL JUST WAITING FOR OUR TURN TO DIE.
WHEN DO WE STOP BEING QUIET?
😡
Elliot Barrett
December 25, 2025 AT 05:05So let me get this straight: flu’s killing more because people got vaccinated? That’s not a win. That’s a failure of the COVID vaccine rollout. If we’d just gotten 60% uptake on the booster, this wouldn’t have happened. We got lazy. We stopped wearing masks. We stopped testing. We told people ‘it’s just a cold’ and now we’re surprised when the system breaks?
Stop acting like this is some new revelation. This was predictable. And we chose to ignore it.
Now we’re just rearranging deck chairs on the Titanic.
Michael Robinson
December 25, 2025 AT 05:16People say ‘it’s just flu.’
But flu doesn’t care if you’re young. Doesn’t care if you’re fit. Doesn’t care if you ‘never get sick.’
It just shows up. And if you’re not ready? It takes you.
We treat COVID like a monster. Flu like a nuisance.
But both kill the same way.
With silence.
And we’re the ones who made that choice.