Medication Heartburn Risk Checker
Find out your heartburn risk from medications
Enter the medications you take regularly to see their heartburn risk level and get personalized safety tips based on clinical evidence.
Millions of people take pills every day to manage chronic conditions - high blood pressure, diabetes, arthritis, infections - but many don’t realize their medication could be causing their heartburn or upset stomach. It’s not just spicy food or stress. Sometimes, the real culprit is the pill you swallowed with a sip of water this morning. If you’ve been dealing with burning chest pain, bloating, or nausea after taking your meds, you’re not alone. And more importantly, you don’t have to just live with it.
Why Your Pills Are Giving You Heartburn
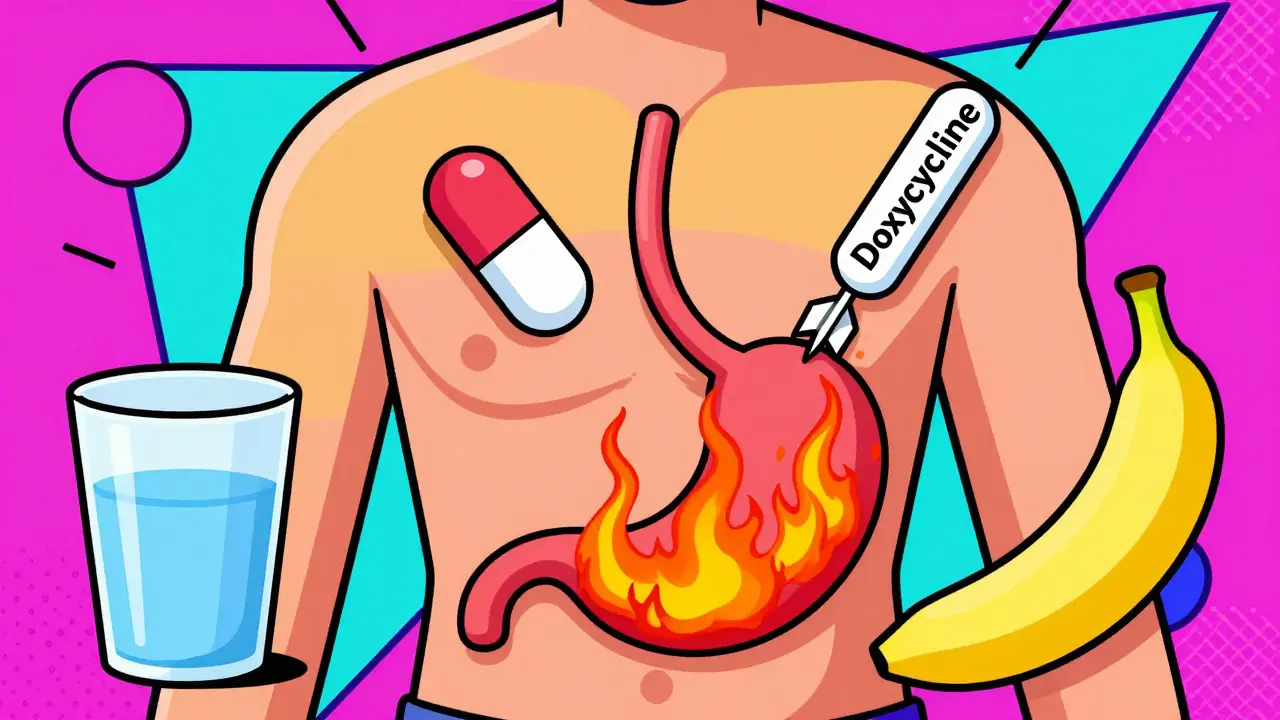
Not all heartburn is the same. When it’s caused by medication, it’s usually one of three things happening in your body. First, some drugs directly irritate the lining of your esophagus or stomach. Second, they relax the muscle at the bottom of your esophagus - the lower esophageal sphincter - letting stomach acid creep up. Third, they ramp up acid production, overwhelming your stomach’s natural defenses. The most common offenders? NSAIDs like ibuprofen and aspirin. These are the go-to painkillers for headaches, back pain, or menstrual cramps. But they block protective chemicals in your stomach lining, making it easier for acid to burn through. About 20-30% of people who take ibuprofen regularly get heartburn. Aspirin isn’t far behind at 15-25%. And if you’ve been taking them for months? Your risk of developing a stomach ulcer jumps from 1-2% to 15-30%. Then there are antibiotics - especially tetracycline and its cousin doxycycline. These are often prescribed for acne or infections. But if you swallow them with too little water or lie down right after, they can stick to your esophagus and cause chemical burns. Up to 12% of people who take doxycycline this way end up with pill-induced esophagitis, with symptoms showing up in just a few hours. Other big players include calcium channel blockers like amlodipine and nifedipine, used for high blood pressure. These drugs relax smooth muscles - including the one that keeps acid down. About 10-20% of people on these meds get reflux. Theophylline, used for asthma, weakens that same muscle by 30-50%, leading to heartburn in nearly a third of users. And let’s not forget metformin, the most common diabetes drug. Around 20-30% of new users get nausea, bloating, or heartburn. But here’s the good news: for most people, these symptoms fade within 2-4 weeks as the body adjusts.Medications That Are Especially Dangerous for Your Esophagus
Some pills aren’t just uncomfortable - they’re risky. Bisphosphonates like alendronate (Fosamax) are used to treat osteoporosis. They’re hard on the esophagus. If you don’t take them correctly - on an empty stomach, with a full glass of water, and stay upright for at least 30 minutes - you could develop severe inflammation or even ulcers. About 5-10% of people who skip these steps end up needing medical care. Potassium chloride, often prescribed for low potassium, can also burn your throat if it doesn’t wash down properly. And quinidine, an older heart rhythm drug, causes reflux in 10-15% of users. These aren’t rare cases. The American College of Gastroenterology says medication-related esophagitis makes up 5-10% of all esophagitis diagnoses. The worst part? Many of these injuries are preventable. A 2023 study from Cleveland Clinic found that 95% of doxycycline esophagitis cases happen because people don’t follow basic dosing rules. Not because the drug is flawed - because the instructions weren’t followed.What You Can Do Right Now to Reduce Symptoms
You don’t have to quit your meds. Most of these side effects can be managed without stopping treatment. Here’s what actually works, backed by clinical data:- Take NSAIDs with food. Eating before or with your ibuprofen or naproxen reduces heartburn by 40-50%. Don’t just swallow it dry - have a snack, a sandwich, or even a banana.
- Drink a full glass of water (8 oz) with every pill. This is non-negotiable for antibiotics, bisphosphonates, and potassium. Water helps flush the pill down before it can irritate your esophagus. Studies show this cuts esophagitis risk by 60-70%.
- Stay upright for 30-60 minutes after taking your meds. No lying down. No napping. No slouching on the couch. Gravity helps keep the pill moving and prevents acid from rising. This simple step prevents 80-90% of pill-induced esophagitis cases.
- Use antacids before NSAIDs. If you know you’re prone to heartburn, take an over-the-counter antacid like Tums or Rolaids 30 minutes before your painkiller. It lowers the chance of symptoms by 30-40%.
- Ask about PPIs if you’re on long-term NSAIDs. Proton pump inhibitors like omeprazole or pantoprazole reduce ulcer risk by 70-80% in people who need daily pain relief. Talk to your doctor - this isn’t something to self-prescribe, but it’s a proven safety net.

What Doesn’t Work - And What Could Make Things Worse
Some advice you’ve heard is misleading - or even dangerous. Don’t take bisphosphonates with coffee, juice, or milk. These interfere with absorption. Only water works. Don’t crush or chew delayed-release pills - they’re designed to dissolve slowly in the intestine, not the esophagus. And don’t take your meds right before bed. Lying flat makes reflux worse, no matter what the pill is. Also, don’t assume heartburn means you’re allergic. It’s not an allergy - it’s irritation. That’s why so many people stop taking life-saving drugs unnecessarily. Research shows 7% of patients quit their meds because of GI side effects, even though simple fixes could’ve helped. Stopping beta blockers cold turkey? That can trigger a heart attack. Stopping metformin? Your blood sugar could spike dangerously. Always talk to your doctor before quitting.When to Call Your Doctor - Not Just Wait It Out
Most medication-induced heartburn is annoying, not dangerous. But some signs mean you need help fast:- Chest pain that feels like pressure, squeezing, or radiates to your arm or jaw - this could be heart-related, not reflux.
- Difficulty swallowing or feeling like food is stuck - this suggests inflammation or scarring in the esophagus.
- Bloody vomit or black, tarry stools - signs of internal bleeding from an ulcer.
- Unexplained weight loss or persistent nausea - could point to something more serious.




Andy Heinlein
January 2, 2026 AT 05:52Man, I was just telling my buddy last week about how ibuprofen wrecked my stomach for months until I started taking it with peanut butter and staying upright. No more burning, no more bloating. Just a damn sandwich and some patience. Life-changing stuff, really.
Todd Nickel
January 3, 2026 AT 05:40The data on NSAID-induced esophagitis is startling, but what’s even more concerning is how rarely primary care providers discuss dosing mechanics with patients. The 2023 Cleveland Clinic study cited in the post-95% of doxycycline cases tied to improper administration-isn’t an outlier; it’s systemic. We treat pills like candy, assuming the bottle instructions are self-evident. But for patients with low health literacy, or those multitasking between jobs and kids, swallowing a capsule with a sip of coffee while rushing out the door isn’t negligence-it’s survival. The burden shouldn’t be on the patient to memorize pharmacokinetic protocols. Pharmaceutical companies and prescribers need to design for human behavior: blister packs with visual cues, voice reminders tied to prescriptions, or even time-release formulations that don’t require 30 minutes of verticality. Until then, we’re just blaming the victim while the system stays unaltered.
Austin Mac-Anabraba
January 4, 2026 AT 10:12Let’s be brutally honest: if you can’t follow basic instructions like ‘drink water’ and ‘don’t lie down,’ you shouldn’t be trusted with prescription medication. This isn’t a medical issue-it’s a cognitive one. People treat their prescriptions like they treat their Netflix passwords-casually, without consequence. The fact that 7% quit life-saving drugs over ‘heartburn’ proves we’ve turned healthcare into a customer service experience. You don’t get to opt out of biology because it’s inconvenient. If your body reacts to a drug, you adjust your behavior, not demand a new formulation. The real tragedy isn’t the side effects-it’s the entitlement.
Phoebe McKenzie
January 6, 2026 AT 06:54Ugh. I can’t believe people still take ibuprofen like it’s candy. You know what else causes heartburn? Ignoring your body. And you know what else causes ulcers? Being too lazy to eat before popping pills. I’ve been on metformin for 5 years and I take it with a protein shake and sit upright for an hour. It’s not hard. If you’re getting heartburn, it’s because you’re doing it wrong. Stop blaming the medicine and start taking responsibility. This isn’t rocket science-it’s basic self-care. And if you can’t manage that, maybe you shouldn’t be in charge of your own health.
Ann Romine
January 8, 2026 AT 01:45As someone who moved from Nigeria to the U.S. and had to navigate this system, I was shocked how little guidance people get. In Lagos, pharmacists explain everything in detail. Here? You get a bottle and a shrug. I once took doxycycline with orange juice because I thought it tasted better. Ended up with esophagitis. I didn’t know it was dangerous until I Googled it at 2 a.m. This post should be mandatory reading for every prescription dispensed. Maybe even printed on the pill bottle itself.
Olukayode Oguntulu
January 8, 2026 AT 09:01Ah, the neoliberal pharmacopeia-where individual compliance becomes the panacea for systemic neglect. The real pathology here isn’t the pill-it’s the capitalist imperative to depersonalize care into a series of behavioral checkmarks. We’ve commodified the body into a machine that must obey the algorithm of dosage protocols, while the pharmaceutical-industrial complex profits from both the disease and the ‘solution.’ The delayed-release doxycycline? A marketing gimmick. The real innovation would be universal healthcare that allows for personalized dosing, not just better packaging. Until then, we’re just rearranging deck chairs on the Titanic… while the iceberg of pharmaceutical greed looms larger.
Heather Josey
January 9, 2026 AT 00:16Thank you for this comprehensive, evidence-based overview. I especially appreciate the emphasis on actionable, non-pharmacological interventions-many patients assume their only options are to suffer or stop the medication entirely. The guidance on timing, hydration, and posture is not only practical but aligns with clinical best practices. I’ve shared this with my patients, and the feedback has been overwhelmingly positive. For those who struggle with adherence, pairing these tips with a simple visual reminder card-provided at the pharmacy-could dramatically reduce complications. Let’s keep advocating for patient-centered education, not just prescription refills.