When a generic drug company wants to bring a new version of a popular medication to market, they usually have to prove it works the same way in the body as the brand-name drug. That used to mean running expensive, time-consuming human trials-giving pills to volunteers, drawing blood every hour, and tracking how the drug moves through the system. But for some drugs, the FDA doesn’t require any of that. Instead, they’ll accept a simple lab test: dissolving the pill in a beaker of liquid and measuring how fast it breaks down. This is called a bioequivalence waiver, or biowaiver.
What Exactly Is a Bioequivalence Waiver?
A bioequivalence waiver lets drugmakers skip human studies if they can prove, using lab tests, that their generic version behaves just like the original. It’s not a loophole-it’s a science-backed rule written into federal regulations (21 CFR 320.22). The FDA decided that for certain types of drugs, in vitro (test tube) data is more reliable than in vivo (in the body) data. Why? Because for these specific drugs, how fast they dissolve in the stomach is the only thing that matters. If two pills dissolve at the same rate under the same conditions, they’ll perform the same in the body.Which Drugs Qualify for a Waiver?
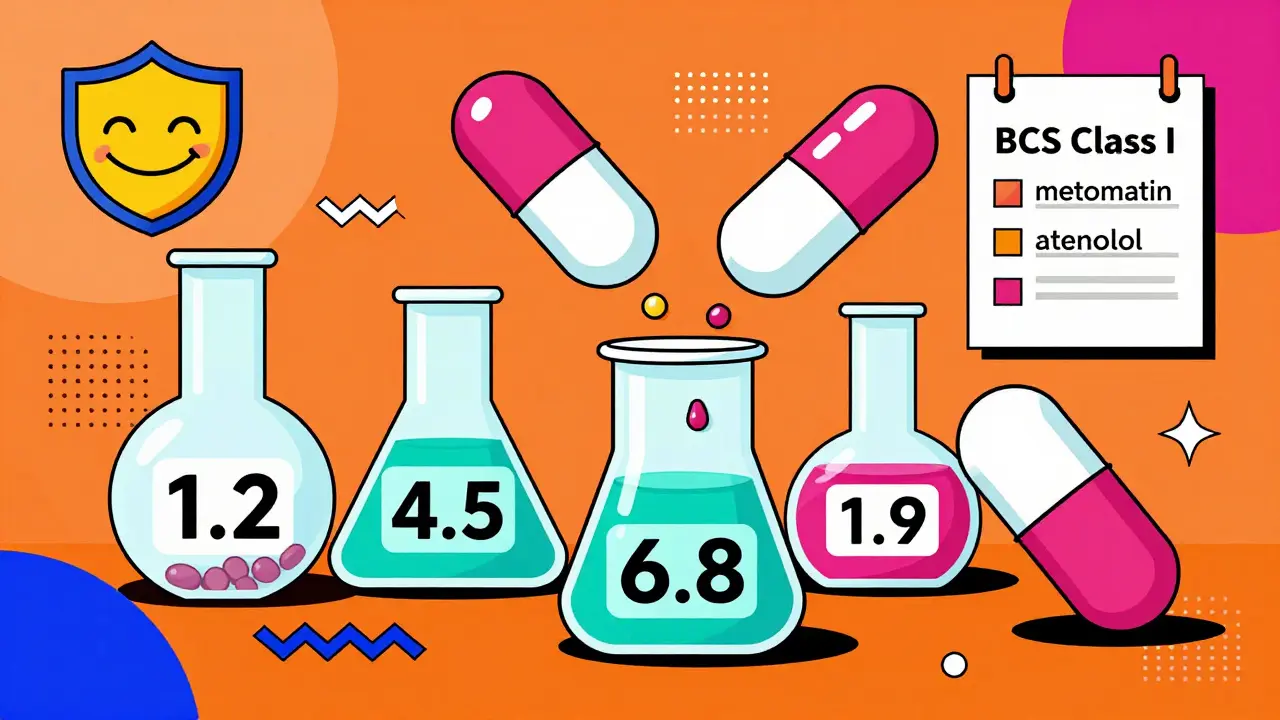
Not every pill can skip human testing. The FDA only allows waivers for immediate-release solid oral dosage forms-think regular tablets or capsules you swallow, not extended-release pills, liquids, or injections. And even then, only if they meet strict criteria based on the Biopharmaceutics Classification System (BCS). The BCS groups drugs into four classes based on two things: how well they dissolve in water (solubility) and how easily they pass through the gut wall (permeability). Only two classes get biowaivers:- BCS Class I: High solubility, high permeability. These are the easiest to qualify. Examples include metformin, atenolol, and ciprofloxacin. If a drug is in this class, and its dissolution profile matches the brand-name version within strict limits, the FDA will likely approve a waiver.
- BCS Class III: High solubility, low permeability. These are trickier. The drug must not only dissolve quickly, but also have the exact same inactive ingredients (excipients) as the brand-name version, and no evidence that absorption changes depending on where in the gut it dissolves.
How Do You Prove Dissolution Is Good Enough?
It’s not enough to just say, “Our pill dissolves fast.” You have to prove it. The FDA requires detailed dissolution testing under three different pH levels that mimic the stomach and intestines: pH 1.2 (stomach acid), pH 4.5 (upper intestine), and pH 6.8 (lower intestine). You test at least 12 tablets or capsules per batch, sampling every 10 to 60 minutes. The key number? The f2 similarity factor. This is a statistical measure that compares how closely your drug’s dissolution curve matches the brand-name drug’s. For a waiver to be approved, the f2 value must be 50 or higher. That means the curves are nearly identical-within a narrow margin of error. If your drug is BCS Class I, you also need to prove it’s highly soluble (dose number ≤ 1 across all pH levels) and highly permeable (at least 90% of the dose gets absorbed). These aren’t guesses-they’re based on published scientific data, often from human studies done years ago for the original drug.Why Does This Matter?
Skipping human trials saves time and money. A single bioequivalence study costs between $250,000 and $500,000 and takes 6 to 12 months. With a waiver, companies can skip all that. One generic manufacturer reported saving $4.2 million and cutting approval time by 8 to 10 months across 12 waiver-approved products. That’s not just corporate savings-it means cheaper medicines reach patients faster. The FDA estimates that in 2022, nearly 18% of all generic drug applications (ANDAs) for solid oral products used a biowaiver. That’s up from 12% in 2018. The result? Generic drugs are hitting the market an average of 7.3 months earlier than they would have otherwise. That translates to over $1.2 billion in annual savings for the U.S. healthcare system.What Doesn’t Qualify?
Biowaivers are not a free pass for every drug. The FDA explicitly excludes:- Narrow therapeutic index (NTI) drugs-like warfarin, levothyroxine, or phenytoin-where even tiny differences in absorption can cause serious harm. The only exceptions are some antiepileptic drugs, where specific guidance exists.
- Modified-release products-time-release pills, patches, or capsules that release drug slowly. These are too complex for simple dissolution testing.
- BCS Class II and IV drugs-those with low solubility. These often need human studies because absorption depends on factors beyond dissolution, like bile salts or food effects.

Why Do Some Waivers Get Rejected?
Even when companies follow the rules, about 22% of biowaiver requests get turned down. The most common reason? Poorly designed dissolution tests. In 35% of rejected applications, the FDA found the test method wasn’t discriminatory enough. That means it couldn’t tell the difference between a good formulation and a bad one. For example, if your dissolution test shows both your tablet and the brand-name tablet dissolve 80% in 15 minutes, but your tablet actually releases the drug slower in real life, the test failed. The method must be sensitive enough to catch small differences in particle size, coating, or binding agents. Another problem? Inconsistent FDA review. A 2022 survey of pharmaceutical companies found that 42% felt the criteria were applied differently across FDA review divisions. One team might accept a waiver for a Class III drug, while another rejects the same submission. That’s why many companies now request a pre-submission meeting with the FDA before spending months on testing.What’s Changing?
The FDA is actively expanding the biowaiver framework. In 2022, they released a draft guidance to include more BCS Class III drugs. In 2023, they launched a pilot program to test whether certain NTI drugs might qualify under stricter conditions. They’re also investing $15 million a year through the GDUFA program to improve in vitro methods and build better models that predict how a drug behaves in the body based on lab data alone. Industry experts predict that by 2027, biowaivers could be used in 25-30% of all generic drug applications-up from 18% today. That’s a big shift. It means more drugs will be approved faster, and more patients will get affordable options sooner.What This Means for Patients
You might never hear the term “bioequivalence waiver,” but you’ll feel its impact. When a generic version of your blood pressure pill or antibiotic becomes available months earlier, it’s often because the manufacturer used a waiver instead of running a human trial. The FDA’s goal isn’t to cut corners-it’s to use science smarter. For drugs where dissolution is the only factor that matters, human testing adds cost without adding safety. That’s why the American Association of Pharmaceutical Scientists says biowaivers have shown over 95% accuracy in predicting real-world performance for BCS Class I drugs. The science is solid. The system works. And for patients, that means more choices, faster access, and lower prices-all without compromising safety.Can any generic drug skip human testing?
No. Only immediate-release solid oral drugs that meet strict criteria based on the Biopharmaceutics Classification System (BCS). Specifically, BCS Class I (high solubility, high permeability) and sometimes BCS Class III (high solubility, low permeability) drugs qualify. Modified-release, injectable, and narrow therapeutic index drugs generally do not.
How much money does a biowaiver save?
A single human bioequivalence study costs between $250,000 and $500,000 and takes 6-12 months. Using a biowaiver can save companies millions over multiple products and cut approval time by 8-10 months per drug.
What’s the f2 similarity factor?
The f2 factor is a statistical measure used to compare how closely the dissolution profile of a generic drug matches the brand-name version. For a biowaiver to be approved, the f2 value must be 50 or higher, meaning the two curves are very similar under standardized test conditions.
Why are BCS Class II drugs excluded from biowaivers?
BCS Class II drugs have low solubility, meaning their absorption depends on more than just how fast they dissolve. Factors like food, stomach pH, and bile salts can greatly affect how much of the drug enters the bloodstream. Because of this variability, in vitro tests can’t reliably predict in vivo performance for these drugs.
Do biowaivers compromise patient safety?
No. The FDA’s biowaiver system is built on decades of scientific research and has been validated in thousands of cases. For BCS Class I drugs, studies show over 95% concordance between in vitro results and actual human performance. The goal is to eliminate unnecessary testing-not risky shortcuts.


Rob Sims
January 23, 2026 AT 07:59Oh great, so now we’re trusting pills to dissolve in a beaker instead of actual humans? Next they’ll let you prove your antidepressant works by watching a YouTube video of someone smiling.
Meanwhile, people are dying because some lab tech didn’t calibrate the pH meter right. But hey, at least the shareholders are happy.
Jasmine Bryant
January 23, 2026 AT 18:26wait so if the pill dissolves fast it’s the same? but what if the coating is different? like the brand has a enteric coating and the generic doesn’t but both dissolve at 80% in 15 min? i feel like this is too simplified
Brenda King
January 24, 2026 AT 19:35This is actually really smart if you think about it
For drugs where absorption is purely about dissolution rate, human trials are just redundant
The science behind BCS Class I is rock solid
And the cost savings? Massive
Patients win, manufacturers win, insurers win
It’s not cutting corners-it’s cutting the noise
Let science do what it’s good at
arun mehta
January 26, 2026 AT 14:31As someone from India where generics save lives daily, this is beautiful
Every rupee saved here means one more diabetic gets metformin
Every month shaved off approval means one more child gets antibiotics before pneumonia sets in
The FDA isn’t being lazy-they’re being *wise*
And yes, Class III waivers are tricky, but the pilot programs are promising
Let’s not fear innovation because we don’t understand it
🙏💊
Tatiana Bandurina
January 27, 2026 AT 04:46You say it’s science, but you ignore the fact that dissolution tests are manipulated.
Companies cherry-pick dissolution media, tweak particle size just enough to pass f2, then change the formulation after approval.
The FDA’s review divisions are inconsistent because they’re understaffed and overworked.
And you think 95% accuracy is good? That’s 1 in 20 patients getting a drug that doesn’t behave the same.
That’s not science. That’s gambling with lives.
And no, I’m not anti-generic. I’m pro-safety.
Keith Helm
January 28, 2026 AT 14:11The Biopharmaceutics Classification System was developed by the FDA in collaboration with academic institutions and validated over decades. The criteria for bioequivalence waivers are not arbitrary. They are based on pharmacokinetic principles and empirical data from thousands of comparative studies. The f2 similarity factor is statistically robust. To dismiss this as a loophole demonstrates a fundamental misunderstanding of pharmaceutical science.
shivani acharya
January 29, 2026 AT 18:51Let’s be real-this whole system is a corporate cover-up.
Big Pharma doesn’t want to spend money on human trials because they’re worried the generics will actually be *better*-and then people will stop buying the brand-name version.
And don’t tell me about BCS Class I-what about all the unpublished studies where generics failed in real patients?
The FDA’s ‘95% accuracy’? That’s a number they cooked up after the lobbyists left the room.
And why is the pilot program only for NTI drugs now? Because someone got sick. Someone always does.
They’ll tell you it’s science. But it’s money. Always money.
And you? You’re just the person taking the pill that might not work.
And they’ll say ‘it passed the beaker test.’
So you’ll keep taking it.
And they’ll keep making billions.
And you’ll never know why you felt worse last month.
Philip House
January 30, 2026 AT 06:12So let me get this straight-America lets a pill dissolve in a cup of acid and calls it science, but we still need 12 different forms to file for a driver’s license?
Meanwhile, China’s doing the same thing but with fewer forms and more efficiency.
This is why we’re falling behind.
It’s not the FDA’s fault-it’s the system.
We’re too scared to trust data unless a human screams about it.
And yet we trust algorithms to pick our dating matches.
Logic is dead.