When your doctor finds a lump in your neck, the first thing they’ll likely order is a thyroid ultrasound. It’s not scary, it’s not painful, and it doesn’t use radiation. But it’s one of the most powerful tools we have to figure out whether that nodule is harmless-or something that needs closer attention.
What Thyroid Ultrasound Actually Shows
Thyroid ultrasound uses high-frequency sound waves to create real-time images of your thyroid gland. Think of it like a sonar scan, but for your neck. The machine sends out sound pulses that bounce off tissues, and the returning echoes are turned into detailed pictures on a screen. This lets doctors see the size, shape, and internal structure of any nodules-something a physical exam simply can’t do.
Most people don’t even know they have thyroid nodules until one shows up on an ultrasound. Studies show that 19% to 68% of adults have them, but only 2% to 21% are found by touch alone. That’s why ultrasound is now the standard first step. It’s cheap-usually $200 to $500 in the U.S.-and it’s safe. No needles, no radiation, no downtime.
The Five Key Features That Matter
Not all nodules are the same. Doctors don’t just look at size-they look at five specific features that help predict cancer risk:
- Composition: Is the nodule mostly fluid (cystic), full of tiny holes (spongiform), or solid? Solid nodules are more concerning.
- Echogenicity: How bright or dark does it look compared to surrounding tissue? Markedly hypoechoic (very dark) nodules are more likely to be cancerous.
- Shape: Is it taller than it is wide? A nodule that’s vertically oriented raises red flags.
- Margin: Smooth edges? Good. Jagged, blurry, or extending beyond the thyroid? That’s a warning sign.
- Punctate echogenic foci: Tiny white dots inside the nodule-these are microcalcifications. They’re one of the strongest predictors of thyroid cancer.
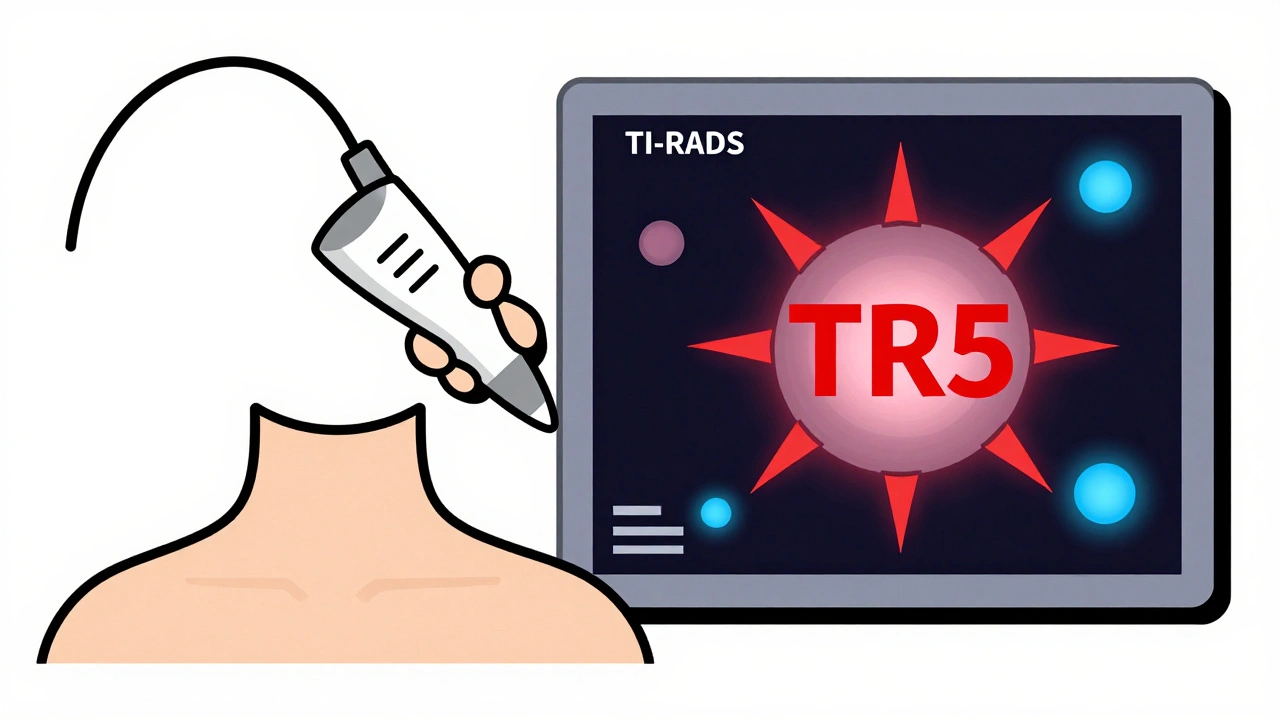
These features aren’t just random observations. They’re the foundation of a system called TI-RADS-Thyroid Imaging Reporting and Data System. Developed by the American College of Radiology in 2017, TI-RADS turns these visual clues into a score. Each feature gets 0 to 3 points. Add them up, and you get a risk category:
- TR1 (0 points): 0.3% chance of cancer
- TR2 (2 points): 1.5% chance
- TR3 (3 points): 4.8% chance
- TR4 (4-6 points): 9.1% chance
- TR5 (7+ points): 35% chance
That’s not guesswork. Large studies have confirmed these numbers. A TR5 nodule isn’t cancer yet-but it’s risky enough that doctors will almost always recommend a biopsy.
Why Ultrasound Beats Other Tests
You might wonder: why not just do a CT scan or MRI? Or a nuclear thyroid scan?
CT and MRI can spot big nodules, but they can’t see the fine details that matter-like microcalcifications or margin shape. They’re also expensive and expose you to radiation. Nuclear scans can tell you if a nodule is “hot” (overactive and almost always benign) or “cold” (underactive, with a 15% cancer risk). But they can’t confirm cancer. Only ultrasound can show the exact features that help decide if you need a biopsy.
And here’s the kicker: ultrasound doesn’t just image the nodule-it guides the biopsy. When a doctor needs to take a sample with a fine needle, they use real-time ultrasound to steer the needle precisely into the nodule. Without it, up to 25% of biopsies come back as “inadequate.” With ultrasound guidance, that drops below 5%.
When You Need a Biopsy-and When You Don’t
Not every nodule needs a biopsy. Size matters, but only when combined with ultrasound features.
For nodules under 5 mm, even if they look suspicious, doctors usually don’t act. The chance of them being dangerous is so low, the risk of over-treatment outweighs the benefit. For nodules 1 cm or larger with suspicious features (TR4 or TR5), biopsy is standard.
For TR3 nodules (moderate risk), biopsy is usually recommended if they’re 2.5 cm or bigger. Why that number? Because research shows thyroid cancers under 2.5 cm rarely spread or cause harm. Many small, low-risk cancers-especially micropapillary types-can be safely watched instead of removed. Studies show 10-year survival rates above 99% with active surveillance.
Even after a biopsy, the story isn’t always over. About 15% to 30% of results come back as “indeterminate.” That means the cells look weird, but not clearly cancerous. In these cases, molecular testing can help. Some tests look for specific gene mutations that tell you if the nodule is likely benign. These tests have cut unnecessary surgeries by half. But even if the test says “benign,” doctors still recommend follow-up ultrasounds every 6 to 12 months. Cancer can grow slowly-and ultrasound catches it early.
The Human Side: Expertise Matters
Ultrasound is powerful-but only if done right. A 2023 study found that radiologists need to perform 200 to 300 supervised scans before they can reliably classify nodules using TI-RADS. Inter-observer variability is real. One doctor might call a margin “ill-defined,” another might say “smooth.” Kappa scores for margin assessment range from 0.45 to 0.67-meaning disagreement happens more often than you’d think.
That’s why accreditation matters. The American Institute of Ultrasound in Medicine requires facilities to prove they get 90% accuracy on 50 consecutive cases. One of the most common mistakes? Skipping the lymph nodes. About 35% of community ultrasounds don’t properly check the neck for swollen lymph nodes-where thyroid cancer often spreads first.
What’s Next? AI and Personalized Risk
Thyroid ultrasound isn’t standing still. In early 2023, a study in Nature Scientific Reports showed a new AI model that improved diagnostic accuracy to 94.2%, compared to 87.6% for traditional methods. The model didn’t just look at the nodule-it analyzed its shape, texture, and how it sat in the gland, using attention algorithms that mimic how human experts focus.
The American College of Radiology is planning a TI-RADS update in 2024 to include data from these AI tools and link ultrasound features to molecular markers. Experts like Dr. Elizabeth N. Pearce predict that within five years, we’ll have personalized risk scores: combining ultrasound findings, gene mutations, and even patient history to give you a single number-your true cancer risk.
That could mean fewer biopsies for low-risk people and faster action for those who truly need it. But the core won’t change: ultrasound remains the first, best, and safest tool we have to look inside the thyroid.
What This Means for You
If you’ve been told you have a thyroid nodule, don’t panic. Most are harmless. But do take ultrasound seriously. It’s not just a picture-it’s a roadmap. It tells your doctor whether to watch, biopsy, or operate. And it’s the only test that can do that without radiation, without pain, and without cost that breaks the bank.
Ask your doctor: What’s my TI-RADS score? What features made them say that? Are the lymph nodes checked? If you’re being advised to biopsy, ask if molecular testing is an option. And if you’re told to just watch it-stick with the follow-up scans. Thyroid cancer grows slowly. Catching it early saves lives.
Is thyroid ultrasound painful?
No. It’s completely painless. You lie on your back with your neck slightly extended. A gel is applied to your skin, and a small probe is moved gently over your neck. It feels like a light massage. No needles, no radiation, no recovery time.
Can ultrasound diagnose thyroid cancer?
No. Ultrasound can only assess the risk of cancer based on nodule features. It can’t tell you for sure if a nodule is cancerous. Only a biopsy-where a small sample is taken and looked at under a microscope-can confirm cancer.
How accurate is TI-RADS?
TI-RADS is the most validated system for thyroid nodule risk assessment. Studies show it correctly identifies cancer risk with 85-90% accuracy when used by trained radiologists. Its strength is in reducing unnecessary biopsies while catching most cancers early.
Do I need a thyroid ultrasound if I have no symptoms?
Only if your doctor finds a nodule-either by touch or incidentally on another scan (like a CT for a different issue). Routine screening for thyroid nodules in people without any signs or symptoms isn’t recommended. Most nodules found this way are harmless.
What happens if my nodule is cancerous?
Most thyroid cancers are highly treatable. The most common type, papillary thyroid cancer, has a 99% 10-year survival rate when caught early. Treatment usually involves removing part or all of the thyroid, followed by hormone replacement. Many patients live normal, healthy lives after treatment.





Francine Phillips
December 2, 2025 AT 08:20My nodule was found on a CT for a sinus infection and I just shrugged it off until my doctor said 'uhhh you should get that checked'
Katherine Gianelli
December 3, 2025 AT 23:19Y’all need to stop panicking about thyroid nodules. I had one the size of a grape and my doc just said 'watch it' - five years later, still chill. Ultrasound is your BFF here. No drama, no needles, just peace of mind. Seriously, breathe.
And if your doc doesn’t check lymph nodes? Find a new one. That’s not optional - it’s the whole damn game.
parth pandya
December 4, 2025 AT 01:47did u know that in india most people dont even get ultrasounds for thyroid nodule unless its huge like a golf ball? we rely on blood tests mostly and if tsh is normal we just say its fine. but i read this and its eye opening. the microcalcifications thing is real. i got mine checked after this post. turned out tr3. no biopsy yet. just watch.
James Kerr
December 4, 2025 AT 16:51So I got my ultrasound last week and my doc said TR4. Felt like my heart dropped. But then she showed me the image and pointed out the tiny white dots - those are the microcalcifications, she said. Honestly? Seeing it made it feel less scary. Like it wasn’t some mystery monster anymore. Just a thing with features. And now I know what to ask about next. Thanks for explaining this so clearly.
Also - gel is cold. Just saying.
Makenzie Keely
December 4, 2025 AT 19:01As someone who’s read every guideline from ACR to ATA - TI-RADS is a game-changer. But here’s what nobody tells you: the radiologist’s experience matters more than the algorithm. I’ve seen the exact same nodule scored TR3 and TR5 by two different clinics in the same city.
Find a facility accredited by AIUM. Ask if they do lymph node mapping. And if you get an indeterminate result? Push for molecular testing - Afirma or ThyroSeq. They’ve cut unnecessary surgeries by nearly half. This isn’t just tech - it’s justice in medicine.
Also - if your doctor says ‘we’ll just monitor’ and doesn’t give you a timeline? Ask for it. ‘Watch and wait’ isn’t passive - it’s active surveillance. You’re part of the team. Own it.
Joykrishna Banerjee
December 5, 2025 AT 21:51Ugh. Another American medical-industrial complex propaganda piece. In India, we treat thyroid disorders with Ayurveda and dietary discipline - no $500 ultrasounds needed. You people are so obsessed with quantifying everything that you’ve lost the art of healing. TI-RADS? More like T-I-R-A-D-S: 'Too Important, Really Arbitrary Diagnostic System.'
And AI? Please. Machines don’t have intuition. They don’t know when a patient is scared. They just spit out numbers. Human touch is dying because of this.
bobby chandra
December 7, 2025 AT 18:09Let’s be real - ultrasound is the unsung hero of endocrinology. No one throws parades for it, but it’s the reason we’re not cutting people open like Thanksgiving turkeys for harmless lumps.
I used to think ‘thyroid cancer’ meant death. Then I met a 28-year-old who had a TR5 nodule, got a biopsy, had half her thyroid removed, and now she’s hiking the Appalachian Trail. 99% survival rate? That’s not a statistic - that’s a second chance.
And if your doc doesn’t explain TI-RADS like you’re a human and not a chart? Fire them. You deserve clarity. Not confusion wrapped in jargon.
shalini vaishnav
December 8, 2025 AT 02:58Why are Americans so obsessed with scanning everything? In India, we don’t waste money on ultrasounds for every little bump. We trust our doctors’ hands and traditional wisdom. This over-medicalization is a Western disease. You turn every mole into a crisis and every nodule into a horror movie. Stop buying into this fear-based healthcare model.
And AI? Ha! What do algorithms know about Indian constitutions? We’ve survived for millennia without your fancy machines.
Myson Jones
December 9, 2025 AT 04:41Thank you for this. I’ve been trying to explain to my sister why she shouldn’t panic after her ultrasound. She thought ‘TR4’ meant ‘you have cancer.’ I showed her this post. She cried. Then she called her doctor and asked about molecular testing. That’s the power of clear information.
Also - I didn’t know lymph nodes were part of the scan. My doctor skipped them. I’m going back with a printed copy of this and asking again. This isn’t just medical advice - it’s advocacy.
vinoth kumar
December 9, 2025 AT 12:28Bro I had a TR3 nodule last year. My doc said ‘watch it.’ I did. Six months later, same size. Now I’m just living. No biopsy, no meds, no drama. This post made me feel like I’m not alone. Thanks for the real talk. Also - if you’re scared, just remember: your thyroid is a butterfly. It doesn’t need to be rescued. Just watched.
And yes, the gel is cold. Always.